INCREASED NUCHAL TRANSLUCENCY
Nuchal translucency (NT) is one of the most well-known markers of fetal health in the 1st trimester. High NT levels are strongly linked to unfavourable pregnancy outcomes.
As experts in this field, we focus on addressing concerns related to increased NT to ensure the well-being of your baby at the earliest opportunity.
Causes of raised nuchal translucency
In some cases where the nuchal translucency is enlarged, several diverse potential issues have been observed in developing fetus. Unfortunately, some of these conditions can be very serious.
The most notable concerns include Down’s syndrome, other chromosomal syndromes, microdeletions disorders, heart defects, diaphragmatic hernia, exomphalos, body stalk anomaly, lethal skeletal problems, neuro-muscular diseases, and specific genetic syndromes like Noonan syndrome.
It’s important to emphasize that most babies with increased NT levels have completely normal outcomes. As fetal care providers, our primary role is to rule out most conditions associated with elevated NT. To provide early reassurance, we employ a combination of early expert ultrasound and advanced NIPT. This approach helps us swiftly assess the baby’s health and offer valuable information to parents during the early stages of pregnancy.

NT 3.3 mm: Increased nuchal translucency above 95th centile
Increased NT: Definition & management
-
The normal nuchal translucency range depends on the gestational week. NT measurements gradually increase as baby grows
-
Normal NT levels 100% safe zone at 11-14 weeks: equal or below 2.2 mm
-
Increased nuchal translucency levels: equal or more than 95th centile
-
Abnormal NT levels: equal or more than 3.5 mm (99th centile)
-
Nuchal translucency percentile chart for normal NT range: link to NT table
-
Cystic hygroma, early fetal oedema, and early fetal hydrops are all conditions that are strongly linked to significantly abnormal NT. See the FAQ session
-
Chorionic Villus Sampling (CVS) is the gold standard for diagnosing chromosomal conditions and microdeletions for babies with abnormal NT (>3.5 mm)
-
CVS is an invasive procedure that requires a needle to be passed through the mother’s tummy. There is a slight risk of miscarriage associated with this test
-
SMART TEST is a comprehensive non-invasive solution designed to provide thorough evaluation and support for babies with elevated NT
-
SMART TEST examines anomalies and diseases that are typically not evaluated through CVS. Notably, this test does not pose a risk of miscarriage
High NT levels: How can we help?
Our Clinical Director, Dr. Fred Ushakov, has had a clinical interest in examining and managing increased Nuchal Translucency (NT) for over two decades. Fred has a wealth of personal experience with Early Fetal Scans and Early Fetal Echocardiography, having worked with more than 1,000 babies with abnormal NT measurements.
Fred has also played a significant role in training fetal medicine professionals, conducting numerous online and in-person training events such as “NT expert” and “Early Fetal Echocardiography.” He provides comprehensive training to our clinical staff for early baby examinations.
Dr. Ushakov understands the complexities associated with increased NT and is sensitive to the stress parents may experience upon receiving such news.
Equally important is our clinic’s expertise in Non-Invasive Prenatal Testing (NIPT). We use clinically approved and extended NIPT that can be beneficial in cases of increased NT, even if a chorionic villus sampling (CVS) has already been performed.
Our SMART TEST offers various options, and we can tailor the test to your specific needs, depending on whether you’ve had already a diagnostic CVS or not.
At the London Pregnancy Clinic, we specialize in fetal non-invasive testing using advanced ultrasound and maternal blood tests for NIPT. We offer various ways to support parents with increased NT, including advanced scans, fetal echocardiography, extended NIPT, and follow-up test planning.
The assistance we provide depends on your specific circumstances: the stage of your pregnancy, the degree of NT increase, any additional findings, and the outcomes of your other tests. We consider whether you’ve had NIPT, CVS, and the type of genetic studies conducted, such as PCR, microarrays, or exome sequencing. Additionally, we assess whether special tests have been undertaken for your baby’s heart.
It’s important to note that we do not offer invasive testing like CVS and amniocentesis in our clinic. These tests can be performed in NHS hospital fetal medicine units at no cost, and these units possess extensive experience in conducting such procedures.
Typically, all babies with nuchal translucency thickness measurements falling within the range of 2.9-3.4 mm are included in this category. You can refer to our chart to determine if your baby’s NT measurement is at or above the 95th centile for its specific age in pregnancy.
When the NT measurement falls between the 95th and 99th centile, you may not qualify for further testing within the NHS. Typically, the NHS plans a scan for your baby around the 20th week (anomaly scan).
Understandably, many parents are concerned about the risks associated with increased NT and wish to exclude associated problems as early as possible.
Our solution for this particular group of patients is the SMART TEST. This specialized approach is an advanced combination of ultrasound and genomic technology. It encompasses two early anomaly scans incorporating early fetal echocardiography and the most advanced NIPT panel available. SMART TEST includes checks for:
- 22 chromosomal aneuploidies (including Down’s syndrome)
- Sex chromosome anomalies (including Turner syndrome)
- Rare chromosomal deletions and duplications <7Mb (including Williams syndrome)
- Nine clinically significant microdeletions (including DiGeorge syndrome)
- 44 different genetic syndromes (including Noonan syndrome)
- 5 inherited monogenic disorders (including cystic fibrosis)
- Majority of severe structural anomalies (including spina bifida)
- Majority of severe heart defects (including transposition of great arteries)
- Accurate fetal sex determination (optional)
Chorionic Villus Sampling (CVS) is the gold standard diagnostic test for elevated NT. CVS is highly effective at excluding potential chromosomal issues associated with increased NT. The test also rules out microdeletions or microduplications, which involve missing or additional copies of genetic material. We strongly recommend parents with babies exhibiting NT measurements greater than 3.5mm consider CVS.
However, it’s important to note that CVS typically does not assess three other crucial components related to increased NT: structural anomalies, heart defects, and monogenic disorders (single-gene diseases). To address these limitations of CVS in a timely manner, we have adapted our SMART TEST to meet these specific needs.
Our “SMART TEST after CVS” is an all-inclusive, one-stop test that encompasses an early fetal scan (early anomaly scan), early fetal echocardiography, and NIPT for selected monogenic conditions (GeneSafe Test). We would recommend proceeding with this test as soon as you receive normal results from the first part of CVS test.
This SMART TEST after CVS performed during one appointment and its checks for:
- 44 different genetic syndromes (including Noonan syndrome and thanatophoric dysplasia)
- 5 inherited monogenic disorders (including cystic fibrosis)
- Majority of severe structural anomalies (including spina bifida)
- Majority of severe heart defects (including transposition of great arteries)
- Accurate fetal sex determination (optional)
This is also a cost-effective solution compared to the full SMART TEST.
Chorionic villus sampling (CVS) or amniocentesis are highly beneficial diagnostic tests that can offer parents reassurance regarding potential chromosomal issues associated with NT. We strongly recommend considering these tests for parents with babies exhibiting NT measurements greater than 3.5mm. However, some parents may opt against these tests due to their invasive nature and the associated risk of miscarriage.
We understand the difficulty of this decision and the uncertainty parents might face concerning their baby’s health. In such cases, they may consider opting for the SMART TEST. This specialized approach represents an advanced blend of ultrasound and genomic technology. It comprises two early anomaly scans, including early fetal echocardiography, along with the most advanced NIPT panel available. The SMART TEST encompasses checks for:
- 22 chromosomal aneuploidies (including Down’s syndrome)
- Sex chromosome anomalies (including Turner syndrome)
- Rare chromosomal deletions and duplications <7Mb (including Williams syndrome)
- Nine clinically significant microdeletions (including DiGeorge syndrome)
- 44 different genetic syndromes (including Noonan syndrome)
- 5 inherited monogenic disorders (including cystic fibrosis)
- Majority of severe structural anomalies (including spina bifida)
- Majority of severe heart defects (including transposition of great arteries)
- Accurate fetal sex determination (optional)
Please note again: the SMART TEST employs a highly advanced NIPT. However, it’s important to understand that this test is not diagnostic in nature. The SMART TEST evaluates probabilities rather than providing a definitive diagnosis.
When it’s not possible to obtain an accurate Nuchal Translucency (NT) measurement during the NHS scan, various factors can contribute to this challenge, including the baby’s position, the position of the uterus, maternal body composition, the quality of the scanner, the expertise of the sonographer, and the stage of gestation.
In such cases, the inability to measure NT can lead to two significant drawbacks: the absence of Combined Screening Test (CST) results and a lack of assessment of the baby’s health. For instance, a baby with increased NT due to heart defects may go unnoticed in these circumstances.
If CST is not possible, you may be referred for the Quad Test, which is a blood test focusing solely on Trisomy 21 (Down syndrome). It’s essential to understand that the Quad Test does not screen for other serious conditions like Trisomy 18 and 13. The detection rate for the Quad Test is relatively low and may miss about 20% of fetuses with Down’s syndrome.
We can offer guidance on how to address this potentially stressful situation and provide you with an Early Fetal Scan. This scan will comprehensively assess all potential factors related to the inability to measure NT. We will perform an NT measurement and evaluate if it falls within the normal range. In our clinic, we do not rely on CST as a screening tool for T21 due to its suboptimal performance, and instead, we use NIPT, considered a much more accurate screening test. Given the significant limitations of the Quad Test, we strongly recommend considering NIPT, which provides comprehensive information about the baby’s health.
Early Fetal Echocardiography or Early ECHO is a special detailed scan for the baby’s heart, which we can perform as early as from 12 weeks.
Our Early ECHO also includes an advanced examination of the baby’s anatomy (brain, face, kidneys and other structures), providing a meticulous top-to-toe examination of the fetus by Early Fetal Scan.
We highly recommend this scan for all babies with increased nuchal translucency (NT) measurements, fetal anomalies, or other unusual findings detected at the 11-13 weeks scan.
We offer second-opinion NT scans. Sometimes, a second opinion on NT measurements becomes necessary when the initial scan encounters challenges due to the baby’s position or movements. This situation may prolong the scan, involving multiple attempts, resulting in different NT measurements. This can leave parents uncertain about which NT value is used for the Combined Screening Test (CST) calculation.
Undoubtedly, highly trained sonographers always follow the protocol, ensuring they select the most precise and highest NT measurement needed for CST Down syndrome chance calculation. However, in certain situations where scan challenges persist, multiple attempts to obtain NT measurements may leave parents feeling unsure. Understandably the parents may choose to repeat the scan and NT measurement for added confidence.
Our goal is to provide assurance that the NT measurement used for CST screening is accurate and the results are reliable. Additionally, with all NT scans we conduct a comprehensive head-to-toe examination of the baby’s anatomy by Early Fetal Scan.
It’s important to note that in our clinic, NT measurements are not utilized for CST; alternatively, you can consider NIPT. NIPT is a highly advanced and accurate screening method. It analyzes the baby’s DNA in the maternal bloodstream and can detect a wide range of conditions, including chromosomal abnormalities like Down syndrome. What sets NIPT apart is its accuracy and reliability; it has a lower chance of false negative and false positive results compared to CST. This means fewer moments of unnecessary worry for the parents.
As part of our routine care, we measure NT thickness during the Early Fetal Scan between 11-13 weeks of pregnancy.
However, it’s important to note that we do not use this measurement to calculate your baby’s chances of having Trisomy 21 (Down’s syndrome). Instead, we rely on Non-Invasive Prenatal Testing (NIPT), which offers a significantly higher detection rate and a lower false positive rate than NT measurement.
In cases where, during any of our Early Fetal Scans, the NT measurement is 3.5 mm or more, we consider this as a cut-off point for referring expecting mothers to a fetal medicine unit. This referral is per NHS guidelines and is intended for further counselling, evaluation and possible invasive testing (CVS).
We would also recommend Early Fetal Echocardiography by Dr Fred Ushakov as soon as possible because your healthcare provider may be unable to offer this test at this early stage, and its performance can be delayed until 16-18 weeks.
Prior to the invention of NIPT (non-invasive prenatal testing), NT thickness was the most effective screening method for trisomy 21 (Down’s syndrome).
About 8-10 years ago, we were actively involved training medical professionals (doctors and sonographers) in performing the NT assessment. As a part of this program, we had created training videos that have been uploaded to YouTube. Overtime, these videos have become one of the most popular NT videos with nearly 700,000 views.
If you click the link below, you will be able to watch these videos, although we would like you to be aware that they are old and have not been updated, because when they were created, 10 years ago, before the era of NIPT, they represented the most advanced information we had about NT measurements.

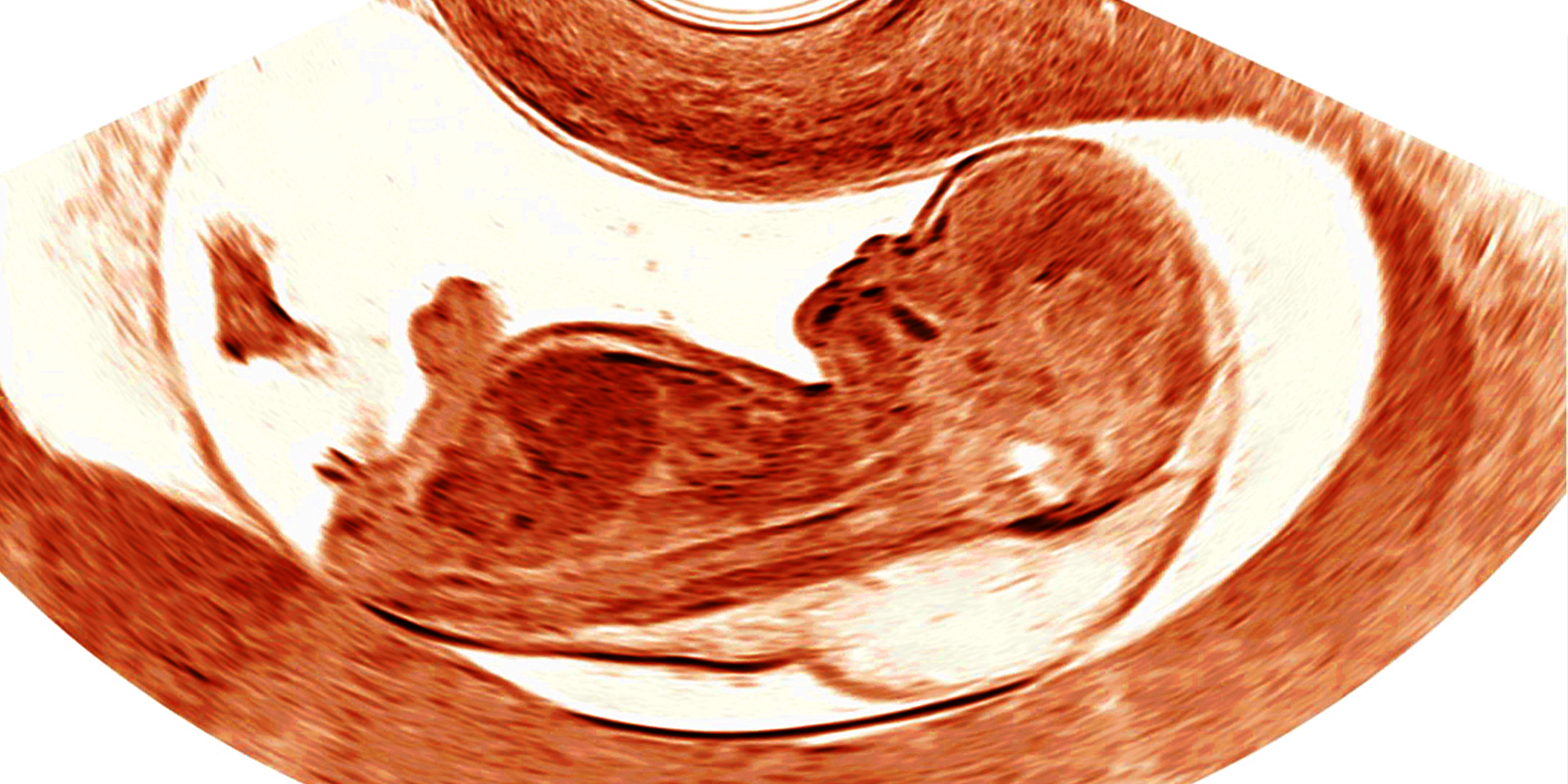
Baby with abnormal NT, cystic hygroma and early hydrops (3D scan)
Yes, the level of increased nuchal translucency impacts your baby’s health outcomes.
NT thickness levels and the chances of having a healthy baby (%)
- normal NT <95th centile – 97%
- 95th-99th centile – 93%
- 3.5-4.4mm – 70%
- 4.5-5.4mm – 50%
- 5.5-6.4mm – 30%
- >6.5mm – 15%
Those are the results of a landmark study led by Prof Nicolaides and his team from King’s College Hospital in 2005, titled “Increased nuchal translucency with normal karyotype,” which sheds light on how NT measurement matters during pregnancy.
This research uncovers a strong connection between a higher NT measurement and potential challenges in your pregnancy journey. These challenges can include chromosomal defects, the possibility of significant fetal anomalies (including heart defects) and a slightly increased risk of miscarriage and fetal loss.
A crucial takeaway from this study is the inverse relationship between NT thickness and the likelihood of experiencing a complication-free pregnancy with a healthy baby. As the NT measurement increases, the likelihood of a smooth pregnancy with a healthy baby may decrease.
If nuchal translucency range is 6.5mm or more the chances of delivering a healthy baby are only 15%. It means that only one in 7 babies with very high NT will be completely healthy.
2.5 mm is the highest value of normal NT at 12 weeks of gestation. NT levels from 2.6 mm are >95th centile for this gestational age (increased NT).
2.7 mm is the highest value of normal NT at 12 weeks of gestation. NT ranges from 2.8 mm are equal to or above the 95th centile for this stage of pregnancy (increased NT).
NT measuring 3.0mm at 12 weeks indicates a slightly increased measurement, placing it between the 95th and 99th centiles. While this increase suggests a slight rise in the chances of chromosomal, genetic, cardiac, or structural problems, it’s important to note that 93% of babies within this range will be born healthy, and only 7% will have issues. If your CST results are low chance (less than 1 in 150), the NHS might not offer you additional tests.
To provide peace of mind and a more comprehensive evaluation, our recommendation is to consider the SMART TEST. The SMART TEST is a comprehensive screening program designed to assess the health and development of your baby during pregnancy. It includes:
Advanced Ultrasound Scans: Our experts will perform early anomaly scans to evaluate various aspects of your baby’s anatomy. This includes detailed assessments of the head, face, heart, abdomen, and other vital structures.
Early Fetal Echocardiography: This specialized ultrasound examination focuses on your baby’s heart, helping to detect any potential cardiac issues early in pregnancy.
NIPT for Chromosomal Anomalies, Microdeletions and Monogenic Conditions (PrenatalSafe Complete Plus): Our SMART TEST features advanced non-invasive prenatal testing (NIPT) that checks also for monogenic disorders, which are single-gene diseases like Noonan syndrome.
The SMART TEST aims to offer you the utmost reassurance and comprehensive insights into your baby’s health, allowing for early detection and timely management of potential issues.
We are truly sorry to inform you that your baby’s NT measurement, which is 6.6mm at 13 weeks, falls within a very high range. Based on clinical evidence, the likelihood of delivering a healthy baby in this situation is only 15-20%. Many babies with such an NT thickness may have chromosomal, genetic, cardiac, or structural issues.
In this challenging situation, our recommendation is to proceed with an Early Fetal Echocardiography, which includes Early Fetal Scan, and to consider the NHS option of CVS (chorionic villus sampling). Additionally, you may qualify for the rapid exome (R21) study, which you can learn more about in our Q&A section.
Another alternative to consider is the SMART TEST, which offers a comprehensive evaluation. Please don’t hesitate to contact us for further information and support.
The optimal scan for a baby with increased nuchal translucency is the Early Fetal Echocardiography, available at our London Pregnancy Clinic starting from 12 weeks. It’s performed alongside an early anomaly scan. These scans serve to rule out most heart defects contributing to increased NT, as well as structural anomalies like exomphalos associated with raised NT. We believe in avoiding any delay and suggest these scans be conducted as soon as possible, ideally before CVS.
While a normal Nuchal Translucency (NT) measurement is reassuring, it’s essential to understand that it doesn’t guarantee protection against serious problems or diseases. Some conditions, like as anencephaly (a severe brain defect), holoprosencephaly (another brain abnormality), gastroschisis (a defect in the abdominal wall), renal abnormalities, and spina bifida (a neural tube defect), can still occur at the same rates as in the general population, even if the NT is normal.
Also, it is important to know that more than half of severe heart defects can appear in babies with normal NT measurements.
That is a valid point indeed. We often discuss increased or elevated nuchal translucency (NT), but what if the NT is low? Does a lower NT pose any risks to the baby or the pregnancy? Is a very low NT (less than 5th centile) considered abnormal?
Here’s a reassuring answer: A low nuchal translucency measurement is not associated with any adverse outcomes for the baby or the pregnancy. In other words, it doesn’t matter how low the NT measurement is. In practical terms, when low NT measurements are factored into Combined Screening Test (CST) calculations, they lead to lower probabilities for conditions like Down’s syndrome and other chromosomal problems.
So, low nuchal translucency levels (NT numbers of around one mm) are brilliant news for you and your baby.
Our response to the frequently asked question, “Is nuchal translucency 1.2 mm at 12 weeks normal?” is a resounding “Yes, it is unquestionably normal!”
The two blood tests, Combined Screening Test (CST) and Non-Invasive Prenatal Testing (NIPT) serve different purposes in Down syndrome screening.
CST, a traditional blood test, measures specific proteins in the mother’s blood—PAPP-A (pregnancy-associated plasma protein-A) and hCG (human chorionic gonadotropin). This test evaluates the likelihood of the fetus having Down syndrome and other chromosomal abnormalities.
On the other hand, NIPT, which stands for Non-Invasive Prenatal Testing, is a more advanced blood test. It detects fetal cell-free DNA present in the mother’s blood, offering a highly accurate assessment of the risk for chromosomal conditions like Down syndrome. Unlike CST, NIPT involves analyzing the fetal DNA fragments circulating in the maternal bloodstream, providing a more detailed and accurate insight into the baby’s genetic health.
NIPT can be performed earlier in pregnancy, typically from around 10 weeks, whereas CST (Combined Screening Test) is conducted later, at 11-13 weeks. The early timing of NIPT allows for earlier insights into the baby’s genetic health, which can be advantageous for expectant parents who seek to obtain information about chromosomal conditions like Down syndrome at an earlier stage in their pregnancy.
The NHS implements “nuchal translucency screening” in two primary ways.
Firstly, it is a component of the Combined Screening Test (CST), where the nuchal translucency (NT) measurement is one of several variables used to assess the risk for chromosomal conditions in the baby.
Secondly, an absolute NT measurement of 3.5mm or more is considered an abnormal value. In this case, it leads to further referral to the Fetal Medicine Unit (FMU) for more extensive evaluation and potentially a chorionic villus sampling (CVS) test to assess the baby’s health.
This approach aims to ensure a thorough assessment and timely intervention if required for the well-being of the baby.
The topic of Nuchal Translucency (NT) is highly significant within the medical field, with approximately 3,000 clinical research publications dedicated to this subject, according to the PubMed database.
Noonan syndrome is a genetic condition strongly associated with increased NT. Noonan syndrome is a monogenic disease (single-gene disorder) and cannot be identified through the current CVS or amniocentesis methods. These tests examine chromosomes using PCR or detect microdeletions through microarrays, unable to identify genetic single-gene disorders. In some instances, material obtained from CVS can undergo an additional check using rapid exome(R21 in the NHS England National Genomic Test Directory). Please refer to the details in the Q&A below.
Alternatively if you wish to undergo a test for Noonan syndrome, but your situation does not meet the R21 eligibility criteria, the SMART TEST is a valuable option. The SMART TEST not only checks for most Noonan Syndrome mutations but can also detect ultrasound features associated with Noonan syndrome.
Rapid prenatal exome sequencing (R21 in the NHS England National Genomic Test Directory) is a specialized genetic test that is conducted in certain high-risk pregnancies where a genetic diagnosis can be incredibly helpful in guiding how the pregnancy is managed.
Currently, at NHS, the R21 test can only be requested by a consultant clinical geneticist after discussing the situation with the local obstetrics team. This test is performed on samples taken during specific prenatal procedures like CVS (Chorionic Villus Sampling) or amniocentesis. The focus of this test is to examine a predetermined panel of genes that are known to be associated with disorders that can become apparent before birth. R21 testing is based on a technology called exome sequencing, which examines a wide range of genes.
In terms of Nuchal Translucency (NT) measurement, R21 testing might be recommended when a fetus shows:
- A Nuchal Translucency measurement greater than 6.5 millimeters.
- The presence of at least one additional anomaly or unusual finding.
- When results from CVS or amniocentesis (PCR and arrays), which are other genetic tests, come back as normal.
It’s important to note that this test examines a specific set of genes, and it is particularly useful for identifying monogenic disorders such as Noonan syndrome. As information about this testing may change over time, it’s a good idea to check for updates in GeNotes when you need the most current information.
Exome sequencing is a valuable genetic testing method that focuses on analyzing the exome, which contains the protein-coding genes in the human genome. These genes provide instructions for building the proteins necessary for various biological functions. Exome sequencing allows for a thorough examination of the exome to identify variations or mutations in the genes that may be responsible for genetic disorders or health conditions.
Exome sequencing can be particularly useful in cases of raised NT during pregnancy. This is because it enables a comprehensive analysis of a wide range of genes associated with genetic disorders. When a fetus presents with an increased NT measurement, it may suggest an underlying genetic issue. Exome sequencing can help identify potential genetic mutations or variations that might contribute to the raised NT.
By examining the exome, clinicians and geneticists can pinpoint genetic mutations that could be associated with conditions such as Noonan syndrome, which is one of the genetic disorders strongly linked to increased NT. Therefore, exome sequencing can provide valuable insights into the genetic factors associated with increased NT measurement, allowing for more accurate diagnosis and personalized management of the condition.
- Diagnostic Genetic Test: The exome test is a diagnostic genetic test that analyzes the exome, which is the part of your DNA responsible for encoding proteins. It’s an invasive test, typically performed through procedures like CVS or amniocentesis.
- Checks Genotype without Phenotype: The exome test focuses on identifying genetic variations (genotype) that may cause specific genetic disorders. It does not evaluate the physical characteristics or anomalies (phenotype) of the baby.
- Invasive: This test involves a needle procedure that carries a small risk of miscarriage.
- No Anomaly Assessment: The exome test does not include the assessment of structural anomalies or physical abnormalities in the baby.
- Holistic Approach: The SMART TEST is a comprehensive screening approach that checks both the physical characteristics (anomalies or phenotype) and genetic variations (genotype) in your baby.
- Selected Monogenic Disorders: It assesses specific monogenic disorders, such as Noonan syndrome, as part of its genetic evaluation. SMART TEST encompasses advanced NIPT, which screens for the most prevalent mutations associated with specific syndromes. It’s essential to know that this test may not identify rare genetic variants (mutations) and can potentially yield false-negative results. Therefore, while it provides valuable insights and information, it may not cover every possible genetic variation.
- Non-Invasive: The SMART TEST is a non-invasive test that uses advanced ultrasound scans and NIPT to evaluate the baby’s health. It does not involve needles and is safer for the pregnancy.
- Probabilities: Instead of providing a definitive diagnosis, the SMART TEST offers probabilities or chances of certain conditions.
In summary, the exome test is a diagnostic genetic test focusing on genotype. At the same time, the SMART TEST takes a holistic approach, checking both genotype and phenotype and is non-invasive, making it a safer and more comprehensive early pregnancy option for many expectant parents. However, the SMART TEST provides probabilities rather than definitive diagnoses, and the number of genetic conditions it currently checks is still limited.
If you’ve had a diagnostic CVS, you might still consider NIPT for monogenic disorders for a broader range of genetic testing.
The SMART TEST is a comprehensive screening option that checks for monogenic disorders, which typical CVS cannot detect. It includes structural assessment of the baby along with fetal echocardiography to exclude congenital heart defects (CHD).
The term “Nuchal test” can be misleading, as it may not specify whether it refers to “nuchal translucency” or “nuchal fold,” which are two distinct measurements in prenatal screening. We believe that, in common usage, the term “nuchal test” often refers to “nuchal translucency.”
When discussing pregnancy and prenatal screenings, it’s crucial to distinguish between different tests and measurements for the well-being of the baby. “Nuchal translucency” and “nuchal fold” are two separate assessments that doctors use during early pregnancy, and they’re not the same thing.
The “nuchal translucency” measurement is obtained through an ultrasound. It involves checking the clear space at the back of the baby’s neck. This test is often conducted around the 11th to 14th week of pregnancy and helps screen for certain chromosomal abnormalities, such as Down syndrome.
On the other hand, the “nuchal fold” measurement is also part of an ultrasound examination. It focuses on the thickness of the tissue at the back of the baby’s neck. Although it’s related to the nuchal translucency assessment, it’s a different measurement that might be used in certain cases and at different stages of pregnancy for various diagnostic purposes.
The term “Nuchal test” might create confusion because it doesn’t specify which of these measurements it refers to—nuchal translucency or nuchal fold. To avoid misunderstandings, it’s best to use the exact and specific terminology when discussing these prenatal screenings. Clarity in communication is essential, especially in the medical field, to ensure everyone understands the exact test being conducted and its implications for the pregnancy.
The term “nuchal fold translucency test” can be confusing due to its mix of terminology, making it potentially unclear in its description. To provide a clear distinction, it’s essential to understand the differences between nuchal translucency (NT) and nuchal fold (NF).
Nuchal Translucency (NT):
- NT is a measurement taken during the first trimester ultrasound scan, typically between 11 and 14 weeks of pregnancy.
- It specifically measures the thickness of the translucent space at the back of the baby’s neck.
- NT is commonly used as a screening tool for chromosomal abnormalities, especially Down syndrome.
- A thicker NT measurement may indicate an increased risk of certain fetal conditions.
Nuchal Fold (NF):
- NF measurement is typically done during the second trimester ultrasound scan, usually between 16 and 24 weeks of pregnancy.
- NF measures the thickness of the nuchal fold at the back of the baby’s neck.
- This measurement is often used to assess the development of the baby and may be a part of the overall evaluation of fetal health.
- NF measurement is different from NT, both in terms of when it’s performed and what it assesses.
So, it’s important to clarify the specific measurement and purpose when discussing this test.
Nuchal Translucency (NT) and Nuchal Fold (NF) represent two separate ultrasound measurements conducted during different stages of pregnancy: NT is typically measured in the first trimester, while NF is assessed in the second trimester. Here’s a detailed comparison of these two measurements:
Gestational Age:
- Nuchal Translucency (NT): Typically measured between 11 and 13 weeks of gestation.
- Nuchal Fold (NF): Usually assessed between 16 and 24 weeks of gestation.
Localization of the finding:
- Nuchal Translucency (NT): Measurement of the clear or translucent space at the back of the fetal neck.
- Nuchal Fold (NF): The thickness or fold of skin at the back of the fetal neck.
Value of Measurements:
- Nuchal Translucency (NT): Considered normal if below the 95th centile for gestational age.
- Nuchal Fold (NF): Considered normal if under 5mm between 16-18 weeks or under 6mm between 18-24 weeks.
Associations:
- Nuchal Translucency (NT): An increased NT measurement is associated with a higher risk of Down syndrome and other chromosomal abnormalities.
- Nuchal Fold (NF): An increased thickness may also be linked to aneuploidy and other fetal abnormalities.
Clinical Use:
- Nuchal Translucency (NT): Primarily utilized for Combined Screening Test (CST) to assess the chance of chromosomal disorders like Down syndrome.
- Nuchal Fold (NF): Although observed during routine ultrasounds, the nuchal fold isn’t specifically used for exact probability calculation, unlike NT.
While there are no specific studies directly comparing NT and nuchal fold for the detection of Down syndrome, NT is widely considered to be a more clinically valuable measurement for assessing the risk of Down syndrome. This is because NT measurements have demonstrated reasonable specificity and sensitivity in numerous clinical settings. Nevertheless, the specific performance of NT and nuchal fold may vary among different healthcare providers and regions. The NT measurement is often preferred due to its established reliability and effectiveness in identifying potential risk factors for Down syndrome.
Cystic hygroma is a fluid-filled sac(s) or cyst(s) that typically develops in the neck or head area of a developing fetus during pregnancy. It is a congenital condition caused by a blockage in the development of the lymphatic system. This results in the accumulation of fluid within the cyst(s), leading to the characteristic appearance of a swelling or lump in the affected area.
Conditions associated with cystic hygroma can include:
- Chromosomal Abnormalities: Cystic hygroma may be associated with chromosomal disorders such as Turner syndrome or trisomies.
- Genetic disorders: Cystic hygroma can be linked to genetic conditions, including Noonan Syndrome.
- Heart Defects: Fetal heart abnormalities can sometimes be linked to cystic hygroma.
- Lymphatic System Disorders: The presence of a cystic hygroma can indicate issues with the development of the lymphatic system, which may lead to lymphedema.
- Other Structural Anomalies: It is possible for cystic hygroma to co-occur with other structural anomalies in the fetus.
It’s crucial to emphasize that discovering cystic hygroma during pregnancy should lead to a thorough evaluation and testing to investigate potential underlying conditions. This may include a specialized anomaly scan, fetal echocardiography, and usually invasive genetic tests.
Skin oedema, also referred to as skin swelling, differs from nuchal translucency (NT). Fetal skin oedema typically indicates a more severe condition. NT is the specific measurement of skin oedema at the back of the fetal neck. Skin oedema involves swelling that can extend to areas like the face, head, chest, and abdomen. This swelling can either be confined to a specific area or spread throughout the body. Generally, when skin oedema is present, the baby might have a serious problem.
Fetal hydrops refers to an abnormal accumulation of fluid in two or more body areas of the fetus. This condition results from various reasons, leading to excessive fluid build-up in spaces like the abdomen, chest, or under the skin.
Although it is not very common, it is possible for a baby at 11-13 weeks to develop hydrops. Unfortunately, first-trimester hydrops often result in a poor outcome for the baby.
Early fetal hydrops is strongly associated with several conditions, such as trisomy 21 (Down syndrome), 45X (Turner syndrome), trisomy 18 (Edwards syndrome), Noonan syndrome, and fetal akinesia deformation sequence, among other causes.
Yes, fluid can be present inside the baby at 11-13 weeks of pregnancy. This is different from increased NT, as the latter specifically measures fluid under the skin at the back of the fetal neck. In cases of fetal hydrops, fluid accumulates in two or more different areas of the baby’s body.
These areas may include around the lungs, known as pleural effusion, around the heart, called pericardial effusion, or inside the abdominal cavity, referred to as ascites. Typically, babies with fetal hydrops also have increased NT measurements.
It’s essential to underscore that detecting fluid in any part of the baby’s body during the first trimester of pregnancy should trigger a comprehensive assessment and testing to explore potential underlying conditions. This assessment may involve a specialized early fetal scan, early fetal echocardiography, and typically CVS (chorionic villus sampling).
Cystic hygroma and nuchal translucency (NT) are distinct from each other. NT refers to a fluid-filled space typically observed behind the fetal neck during a first-trimester ultrasound. Unlike cystic hygroma, NT is considered a normal structure when its measurement falls within the typical range.
The key differences between cystic hygroma and nuchal translucency (NT) are as follows:
Location: Cystic hygroma is typically located around the neck or head region of the fetus, while NT refers to the measurement of fluid specifically at the back of the fetal neck during an ultrasound scan.
Nature: Cystic hygroma is a physical abnormality characterized by a fluid-filled cyst(s), while NT is a measurement of the thickness of the fluid in the nuchal region.
Diagnostic Significance: Cystic hygroma is often identified during prenatal ultrasound and may indicate an increased risk of chromosomal or genetic abnormalities or other fetal conditions. NT measurement is used to assess the risk of certain chromosomal abnormalities, such as Down syndrome.
It’s important to understand that the current version of SMART TEST, which includes GeneSafe or PrenatalSafe Complete Plus by Eurofins, has one of the most comprehensive monogenic NIPT panels available. However, it may not cover all genetic conditions associated with an increased NT. This limitation arises from the constraints of current genomic technology and the variability of mutations, as well as the constant discovery of new genes related to specific conditions.
Here are a few examples of conditions that may not be detectable by SMART TEST:
Spinal Muscular Atrophy (SMA): SMA is a well-known condition associated with an increased NT. However, GeneSafe cannot screen for SMA. To check for this condition, you can add the UNITY Carrier Screen (another type of sgNIPT), which includes SMA in its assessment.
New or Rare Mutations in Noonan Syndrome: Noonan syndrome can result from mutations in various genes. While GeneSafe covers the majority of pathogenic variants, it may not include all of them. For instance, newly described and rare LZTR1 mutations are not included in the panel.
Conditions like Kabuki Syndrome: Some genetic conditions, such as Kabuki Syndrome, are not part of single-gene NIPT panels. While GeneSafe can not identify mutations in genes like KMT2D and KDM6A, which can cause Kabuki syndrome. SMART TEST can reveal fetal anomalies, including heart defects and other issues, through the Early Fetal Echocardiography and Early Fetal Scan included in the test. However, the specific genetic cause of the fetal condition will remain undiscovered by NIPT.
To address these limitations of single-gene NIPT, it’s possible to consider an exome test on fetal DNA obtained from an invasive sample (as discussed in the Q&A on exome – R21). This way, you can explore a broader spectrum of genetic information and make more informed decisions about your pregnancy.
Please be aware that the London Pregnancy Clinic specializes in non-invasive fetal testing, which includes ultrasound scans and NIPT. We do not conduct invasive procedures like CVS or amniocentesis. However, if you require invasive testing, we can provide referrals to other healthcare providers in London who offer these services. Your care and well-being during your pregnancy are our top priorities, and we are here to assist you in finding the most appropriate resources for your specific needs.
Yes, it works. Since the early 1990s, medical experts have recognized the significance of NT measurements at 10 weeks. Recent studies have not only reaffirmed this importance but have also highlighted the strong link between increased NT at 10 weeks and conditions like Down’s syndrome and other chromosomal anomalies.
Keep in mind that at 10 weeks, the baby is much smaller compared to the 11-14-week period. Therefore, specific NT range charts have been developed for 9-11 weeks, and these early NT thickness ranges are included in our 95th centile chart. It’s important to note that, for a significant number of healthy babies, increased NT at 10 weeks will naturally resolve, and subsequent scans at 11-13 weeks may show absolutely normal measurements. In these cases, if the results of genetic testing like NIPT or CVS are normal, the outlook for the baby is typically good.
At the London Pregnancy Clinic, our experienced clinicians assess the appearance of NT during the 10-Week Scan. If they observe increased NT, they will measure it and comment in the report if the measurements exceed the 95th percentile. This information is invaluable for parents, primarily because diagnostic tests like CVS can only be performed from 11 weeks onwards, and at this early stage, only NIPT is available. Our fast-track NIPT can provide essential insights into the most common chromosomal anomalies associated with increased NT, including Down syndrome (T21), Edwards syndrome (T18), Patau syndrome (T13), and Turner syndrome (45X). This early information can be a crucial step in ensuring your baby’s well-being.
You can learn more from our dedicated page Nuchal Translucency at 10 weeks.
Nuchal translucency (NT) refers to measuring the clear space at the back of the baby’s neck during the first trimester of pregnancy. The terms mentioned: increased NT, high NT, elevated NT, thickened NT, NT above the range, and abnormal NT—are often used interchangeably. However, they might convey slightly different nuances in context:
- Increased NT: Indicates a measurement that is higher than what is considered typical for the gestational age of the fetus, usually 95th centile.
- High NT: Suggests a measurement that exceeds the normal or average range for that stage of the pregnancy; it is unclear if it is 95th or 99th centile.
- Elevated NT: Similar to “increased” or “high,” referring to a measurement outside the expected range (>95th centile).
- Thickened NT: Another way of describing an NT measurement that is larger than the norm for that stage of pregnancy. Sometimes, 3.0mm is used as a cut-off. We do not recommend using this term and range.
- NT above the range: Denotes a measurement that surpasses the established normal range for that specific gestational period, which can be 95th or 99th centiles.
- Abnormal NT: Generally refers to an NT measurement that is not within the expected or standard range for that stage of pregnancy. We believe that this term must be reserved to NT 3.5mm or more (>99th centile).
While these terms may be used somewhat interchangeably, they all indicate the same fundamental issue: an NT measurement that is not within the normal range for the gestational age (>95th or >99th centiles). NT thickness of 3.5mm and more represents an abnormal range.
“Transnuchal scan” is not a widely recognized or commonly used term in medical terminology. The combination of the words “Transnuchal Scan” seems to be a blend of “trans” (indicating translucency) and “nuchal.” This suggests that it might have been coined to describe nuchal translucency.
The term “Transnuchal Scan” can be misleading because it doesn’t specify whether it’s referring to nuchal translucency or nuchal fold measurements, which are different. To avoid confusion, it’s best to use the specific terms “Nuchal Translucency (NT) scan” for the clear space at the back of a baby’s neck or “Nuchal Fold scan” for the measurement of the skin fold at a slightly different location during prenatal screenings.
“Lucency” in medical terms refers to a clear or translucent area often seen in X-ray images created by radiography. It’s not commonly used in ultrasound imaging. The term “nuchal lucency” isn’t precisely accurate when discussing prenatal ultrasound. Instead, healthcare professionals use the term “Nuchal Translucency” (NT) to refer to the clear space at the back of a baby’s neck visible during an ultrasound in early pregnancy.
“Nuchal Translucency” specifically describes the clear space seen in an ultrasound, and it’s a crucial measurement to screen for certain conditions. It’s important for parents to be aware of this term and its significance during early pregnancy screenings, as it provides valuable information about the baby’s health.
Therefore, the term “nuchal lucency” is not a correct or commonly used expression. Using “nuchal lucency” might cause confusion as it doesn’t accurately represent the intended meaning and could lead to misunderstandings. Therefore, it’s recommended to stick to the established term “Nuchal Translucency” to avoid any confusion and ensure clear communication between healthcare providers and parents.
Many internet searches for “nuclear translucency” are the result of smartphone autocorrection, which actually refers to “nuchal translucency.” If your smartphone’s autocorrect has brought you here, you’ve landed in the right place. This page is dedicated to NT and its significance for your baby’s well-being. It’s important to note that there’s nothing “nuclear” about nuchal translucency. However, in some unfortunate cases, the severity of the news associated with NT findings can be so impactful that it may feel like a “nuclear” event for parents.


