Early Fetal Scan Explained

Early Fetal Scan Explained

Miss Shaz Khojasteh on why scanning at 12-16 weeks is important for Mothers.
Published
Tags
The early stages of pregnancy are a time of wonder and crucial development. At London Pregnancy Clinic, we offer a thorough Early Fetal Scan to nurture early prenatal care and provide expectant parents with detailed insights into their baby’s early development.
When I joined the London Pregnancy Clinic, the importance of the Early Fetal Scan became vividly clear through experiences with expectant parents. This critical scan, offering a glimpse of their baby’s developing heartbeat and form, goes beyond just a medical check-up; it’s an early, reassuring window into the baby’s well-being and a vital tool for detecting potential anomalies. At the clinic, we do more than just scans; we provide a journey of reassurance, care, and emotional support, making each early pregnancy scan a crucial, heartwarming step in the beautiful journey of parenthood.
The Basics of Early Fetal Scan
Performed between the crucial 12-16 week mark, the Early Fetal Scan is an essential part of your prenatal care regimen. It provides a detailed look at your baby’s development, including their physical structure, heart rate, and movement. This scan also assesses the health of the placenta, which is vital for your baby’s nourishment and growth.
Importance of Early Fetal Scan
Early Detection of Anomalies: This scan plays a critical role in the early detection of over 100 different structural abnormalities. These include severe heart defects, early brain anomalies, spina bifida, lethal skeletal dysplasias, and other serious structural conditions. The scan even has the precision to detect minute details such as missing fingers, providing a comprehensive view of the baby’s development.
Beyond Structural Analysis: While this scan is adept at identifying structural abnormalities, it’s important to note that ultrasound alone cannot detect chromosomal conditions. A baby may appear structurally normal but still have chromosomal defects like Down’s syndrome (Trisomy 21). If you haven’t already done this with an earlier pregnancy scan like our 10 Week Scan, we strongly recommend doing a non-invasive prenatal test (NIPT). Complementing our 12-16 week pregnancy scan with NIPT will help identify such chromosomal syndromes and is currently the best screening option available and it is part of our signature Ultrasound plus NIPT Dual Approach.
12-16 week Ultrasound Images of the baby
Here are some of the pictures you can get of your baby at 12 to 16 weeks of pregnancy using our state-of-the-art Voluson ultrasound machine.
-

13 weeks of pregnancy
Captured via ultrasound at 13 weeks, this image showcases the incredible clarity of our scanning technology, revealing even the tiny fingers of the baby in amazing detail.
-

14 weeks of pregnancy
3D ultrasound image of a 14-week-old fetus, showcasing clear features and a serene pose often described by patients as the ‘sucking of the thumb in the womb’.
Your Experience with Early Fetal Scans
We achieve the best results by combining external (transabdominal) and optional internal (transvaginal) scans, adapting to factors like womb position, fetal position, and maternal abdominal wall thickness. While our high-resolution transducers often suffice with transabdominal scans, around 10% of women with a retroflexed uterus may benefit more from a transvaginal scan. We ensure you’re fully informed and comfortable with your scanning choices. You can read more about what to expect during a pregnancy scan here.
Your frequently asked questions about Early Fetal Scan:
When should I do this early pregnancy scan?
Schedule Scan at 14-16 Weeks: Post 10 Week Scan and NIPT for a detailed anomaly check, as the baby’s advanced development at this stage allows for more comprehensive screening.
Early Scan at 12-13 Weeks for First-Time Checks: If no early anomaly scan was performed by 10 weeks, opt for this ultrasound scan combined with NIPT for effective Down’s syndrome screening.
Address Unclear NHS 12 week scan Findings with Echocardiography: For inconclusive first trimester results, like increased NT, our Early Baby Heart Scan provides an in-depth heart evaluation and a thorough early baby scan.
Can an early fetal scan detect all fetal anomalies? While no single test can diagnose all fetal anomalies, our early baby scan at London Pregnancy Clinic identifies many, particularly severe abnormalities that might lead to disability or require early intervention. However, certain anomalies, especially those affecting late brain or heart development, may not be detectable at 12-13 weeks. We recommend follow-up scans at 20-22 weeks and 28-29 weeks for comprehensive monitoring, alongside maintaining your NHS scan schedule, to ensure the best care for your pregnancy
-
London Pregnancy Clinic Scan Overview
London Pregnancy Clinic Scan Overview
-
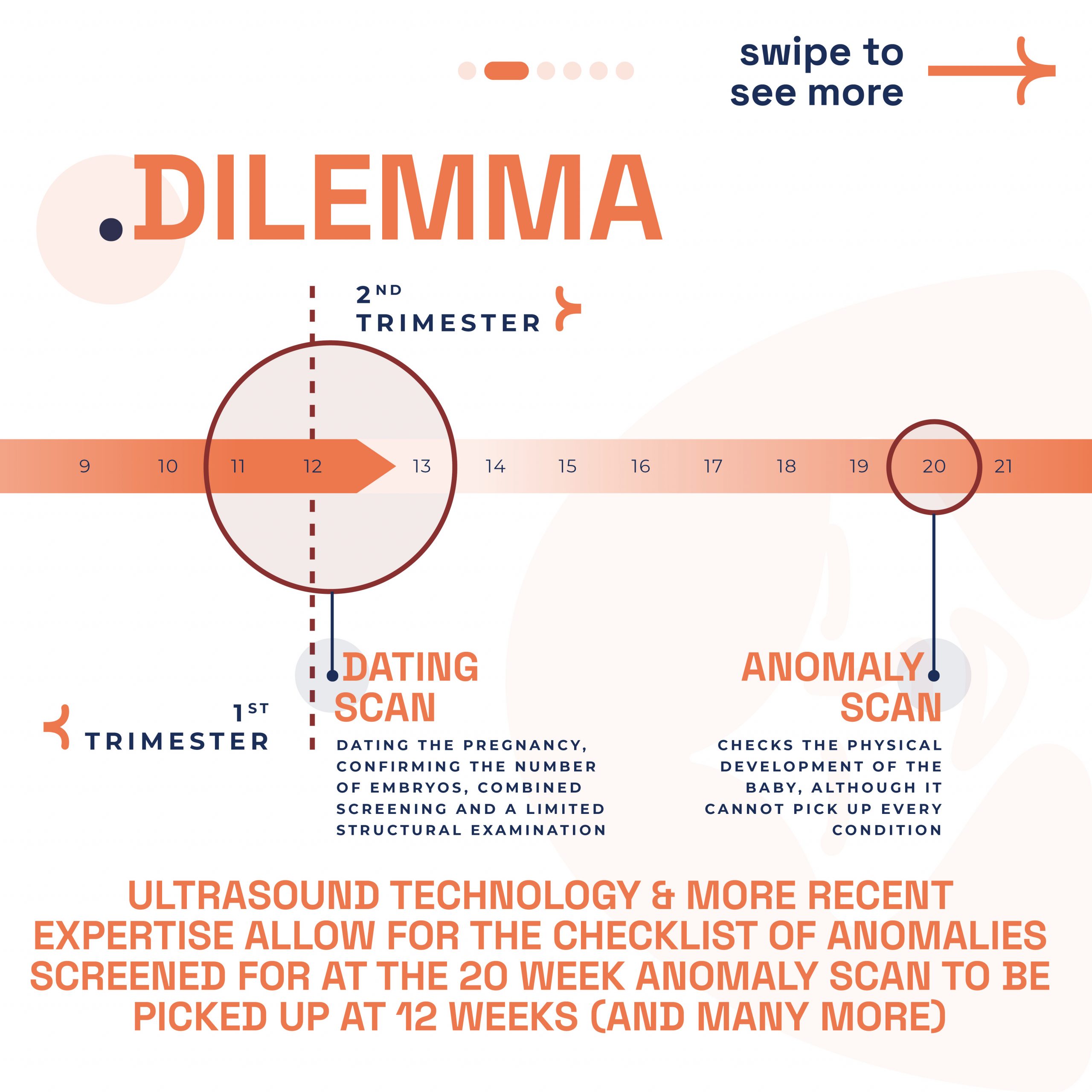
Why we need 12 to 16 week private pregnancy scan?
Why we need 12 to 16 week private pregnancy scan?
-
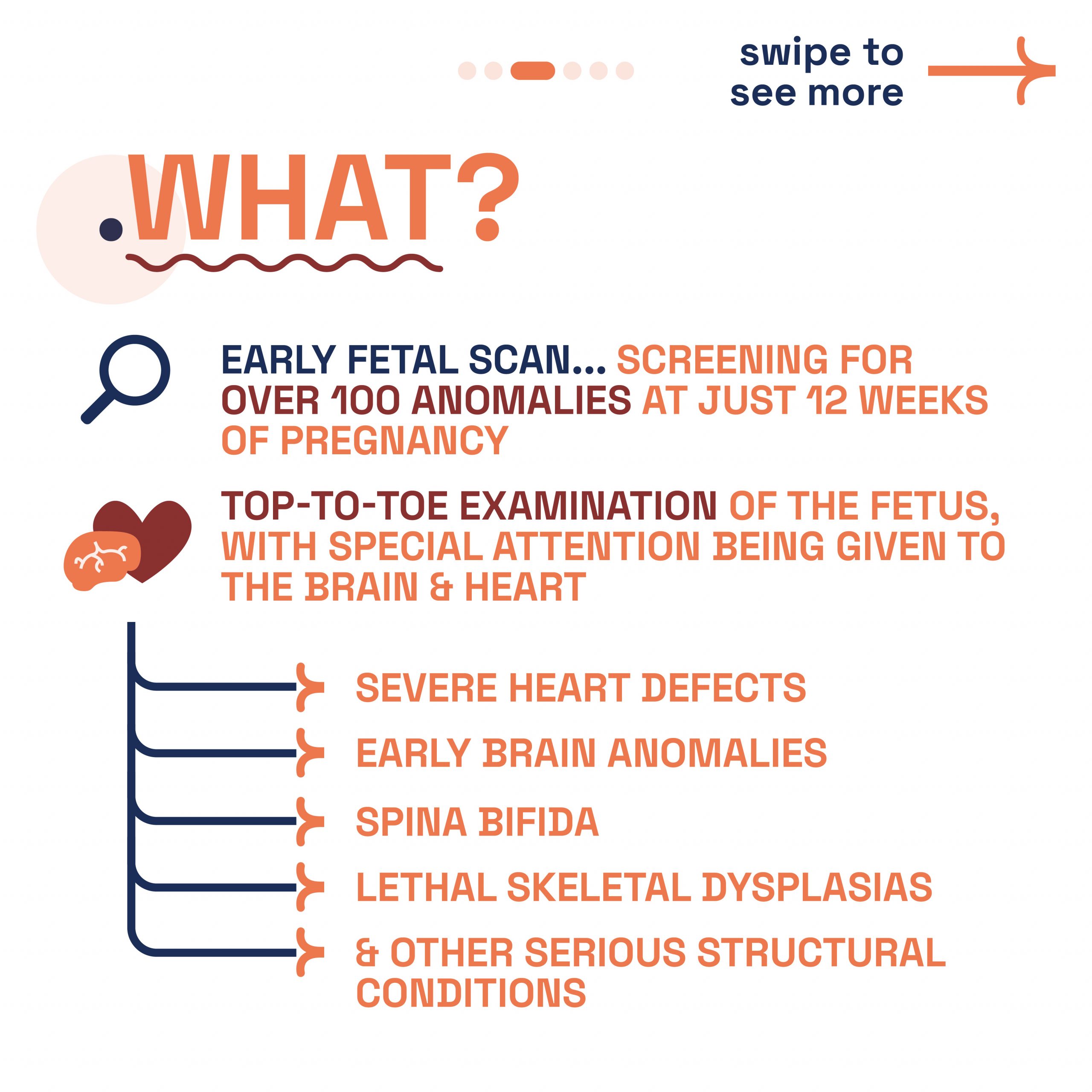
What is Early Fetal Scan?
What is Early Fetal Scan?
-
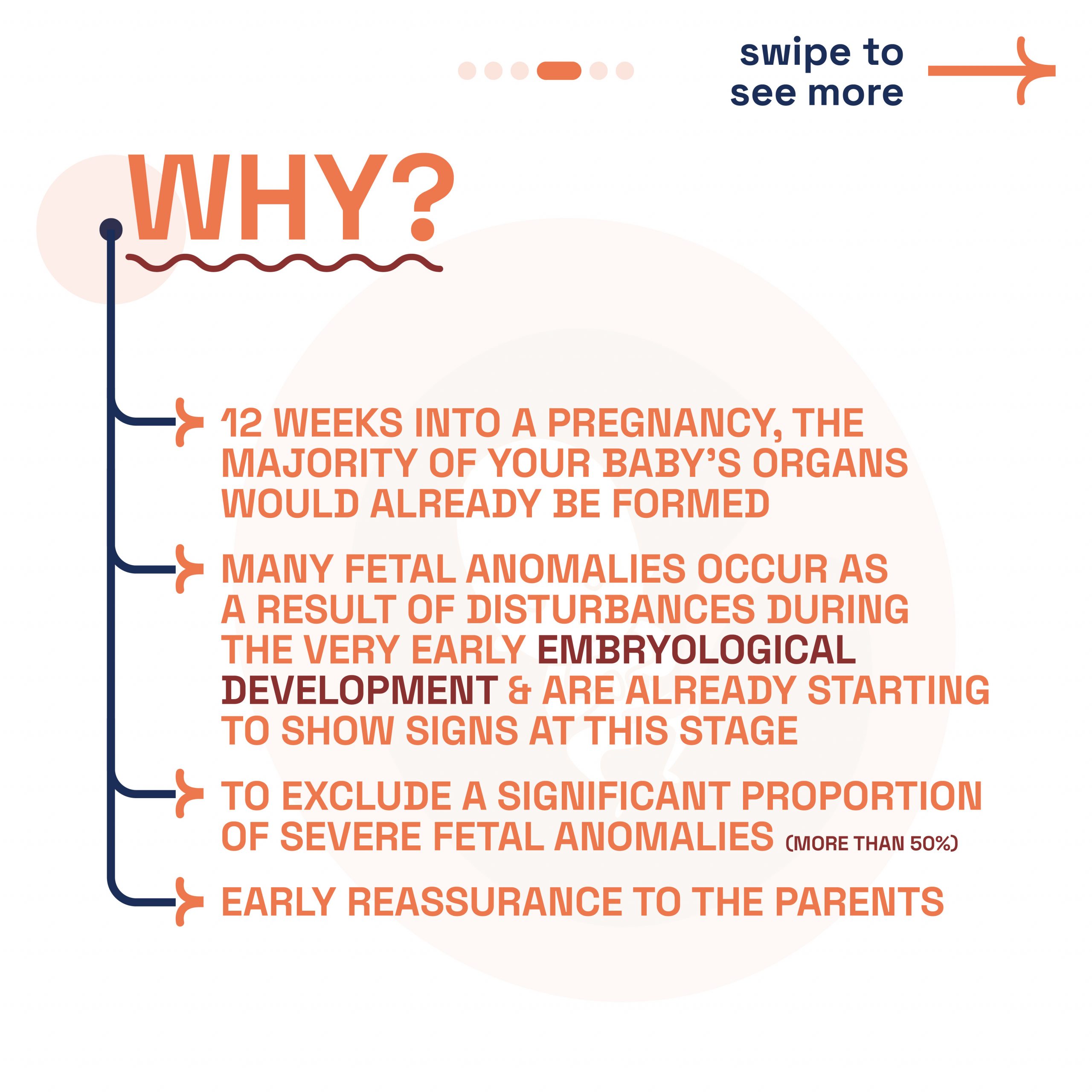
Why do Early Fetal Scan?
Why do Early Fetal Scan?
-
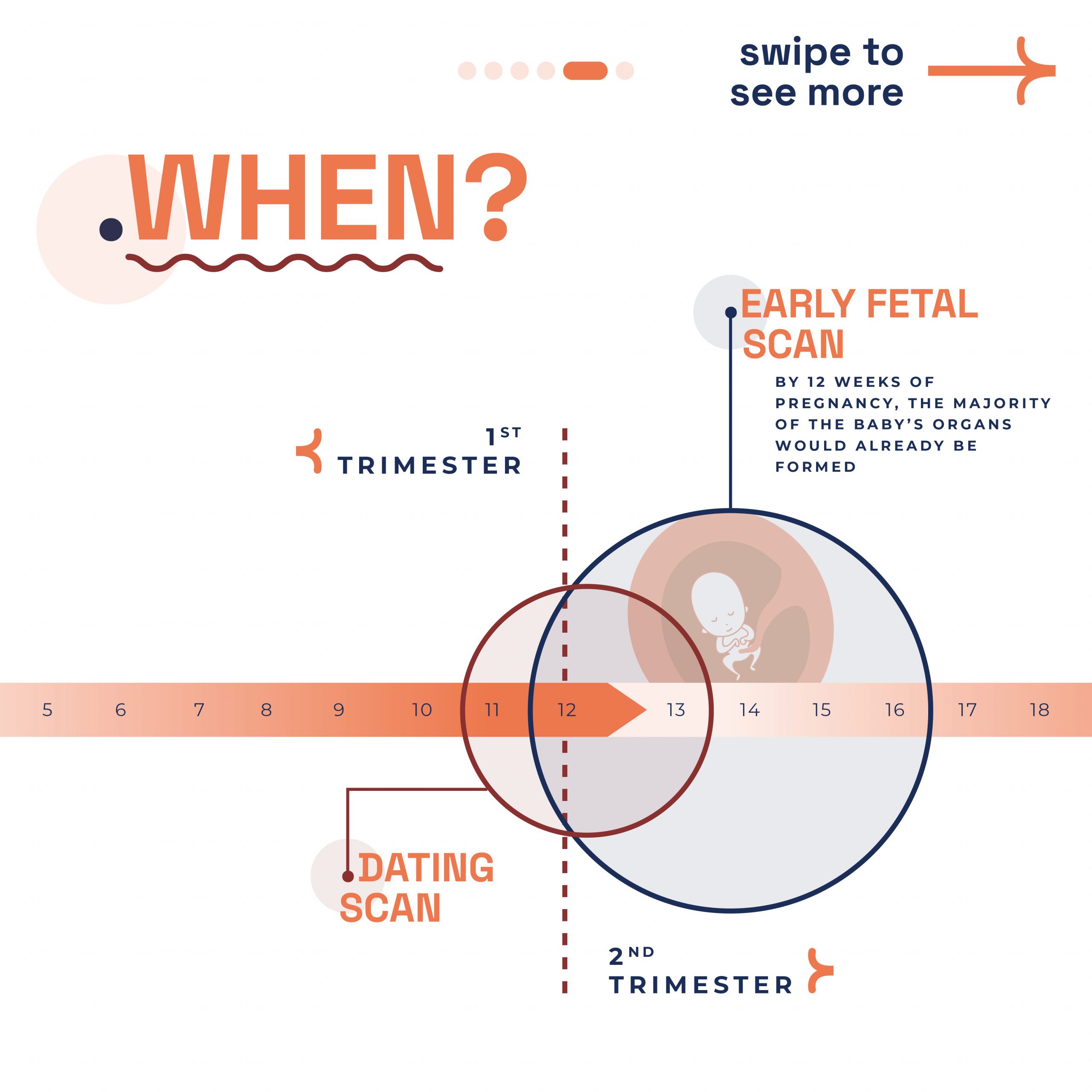
Best time for EF Scan?
Best time for EF Scan?
-
Get in touch
Get in touch
Conclusion
The Early Fetal Scan is a pivotal part of your pregnancy journey, offering invaluable insights for peace of mind and informed decision-making. At London Pregnancy Clinic, we’re committed to providing detailed, compassionate care during this vital phase of your pregnancy.