The Fertility Show London

LPC at Fertility Show 2024
-
Published
-
Last Modified
Tags
London Pregnancy Clinic (LPC) is excited to share our experience exhibiting at the Fertility Show 2024 in Olympia, held on 18-19 May. This prestigious event brought together top fertility experts, clinics, and support groups, offering invaluable insights and support to those on the path to parenthood. LPC was thrilled to be part of this inspiring event, connecting with attendees and sharing our expertise in prenatal care.
Fertility Show 2024 at Olympia was a remarkable event that provided a comprehensive platform for individuals and couples looking to start or grow their families. As first-time exhibitors, LPC was honoured to participate in this two-day event, which featured over 70 exhibitors, including leading fertility specialists, clinics, and support groups.
Connecting with Attendees
At the Fertility Show, we had an amazing time, meeting and connecting with so many incredible professionals in the field. Our stand was buzzing with activity as we shared insights about our comprehensive prenatal services and discussed the latest advancements in fertility care. The event was an incredible opportunity for LPC to engage directly with prospective parents. Our team was on hand to answer questions, provide guidance, and offer reassurance to those embarking on their fertility journey. We were thrilled to meet so many individuals and couples seeking to expand their families.
Expert Insights and Panels
It featured a series of expert panels and seminars covering a wide range of topics, from the latest advancements in IVF to holistic approaches to fertility. LPC’s representatives attended sessions led by renowned fertility specialists and participated in discussions about the latest trends and techniques in reproductive medicine.
One of the standout features of the show was the Fertility Support Hub. This dedicated space offered attendees the chance to meet with nurses, counsellors, and workplace support teams. LPC’s own team of specialists provided one-on-one consultations, helping attendees navigate their options and make informed decisions about their fertility treatment.
Special Acknowledgments
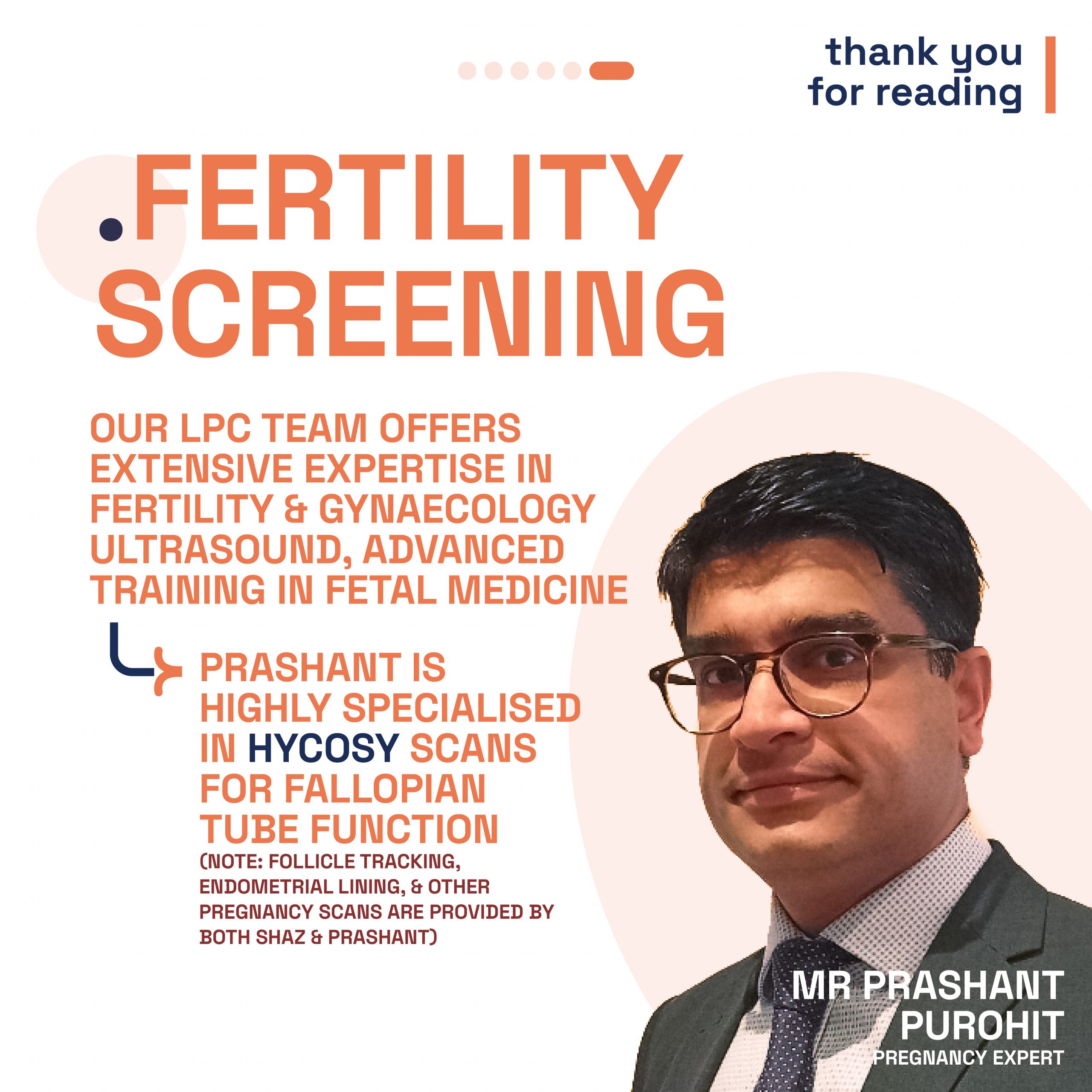
A special shout out to our dedicated obstetrics and gynaecological team Shaz Khojasteh, Diane Nzelu, Prashant Purohit, and Molly Payne. Their expertise and passion were truly inspiring to all who visited our stand. Your commitment to advancing fertility and prenatal health is what makes us stand out.
Our team worked hard to set up and design the space to be welcoming and homey, and a lot of you loved it! Our totes were a big success and were taken very fast too.
Our Services
Here at LPC we offer comprehensive services designed to support you throughout your fertility and pregnancy journey. Our mission is to provide a reassuring experience through our extensive expertise and ultrasound technology.
Preconception
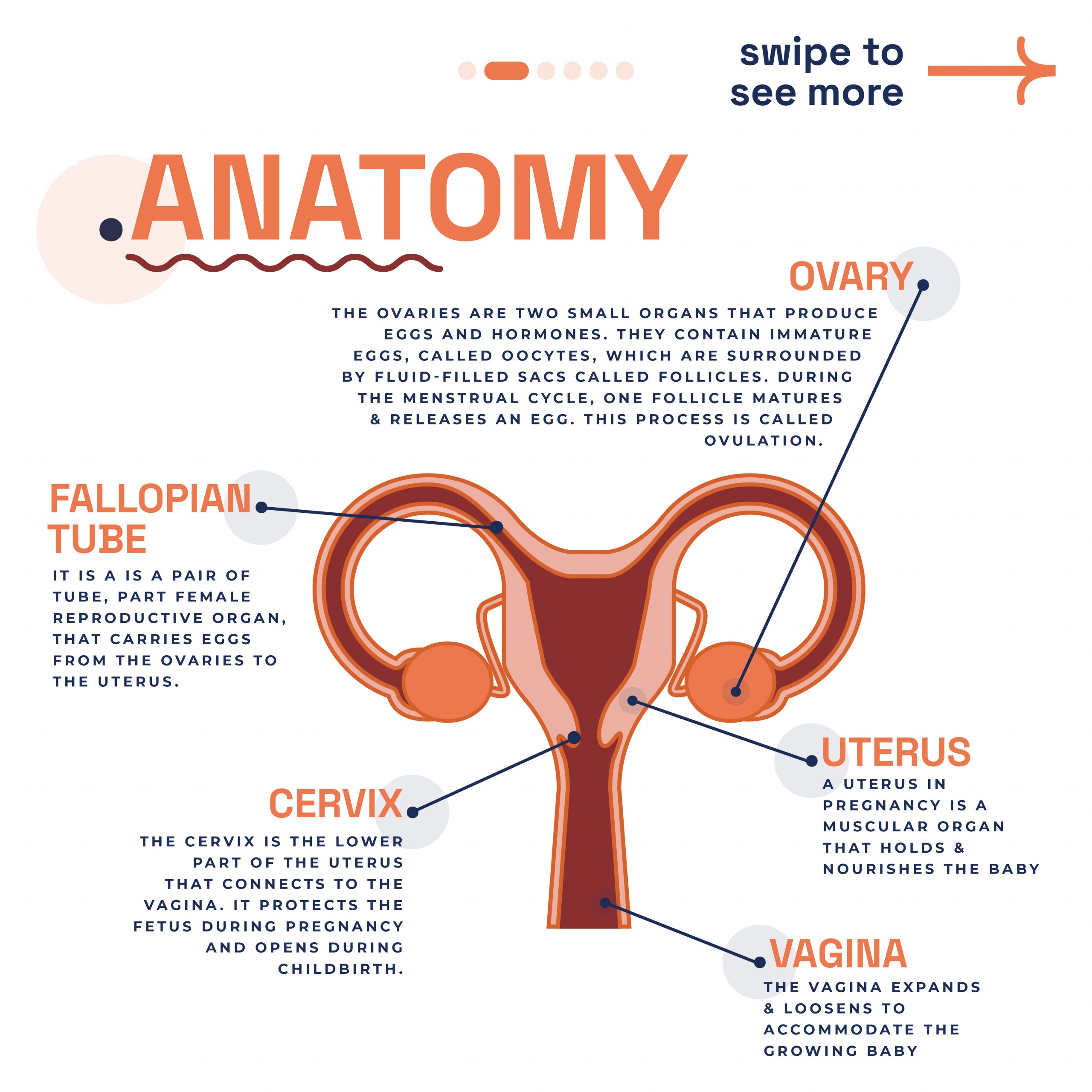
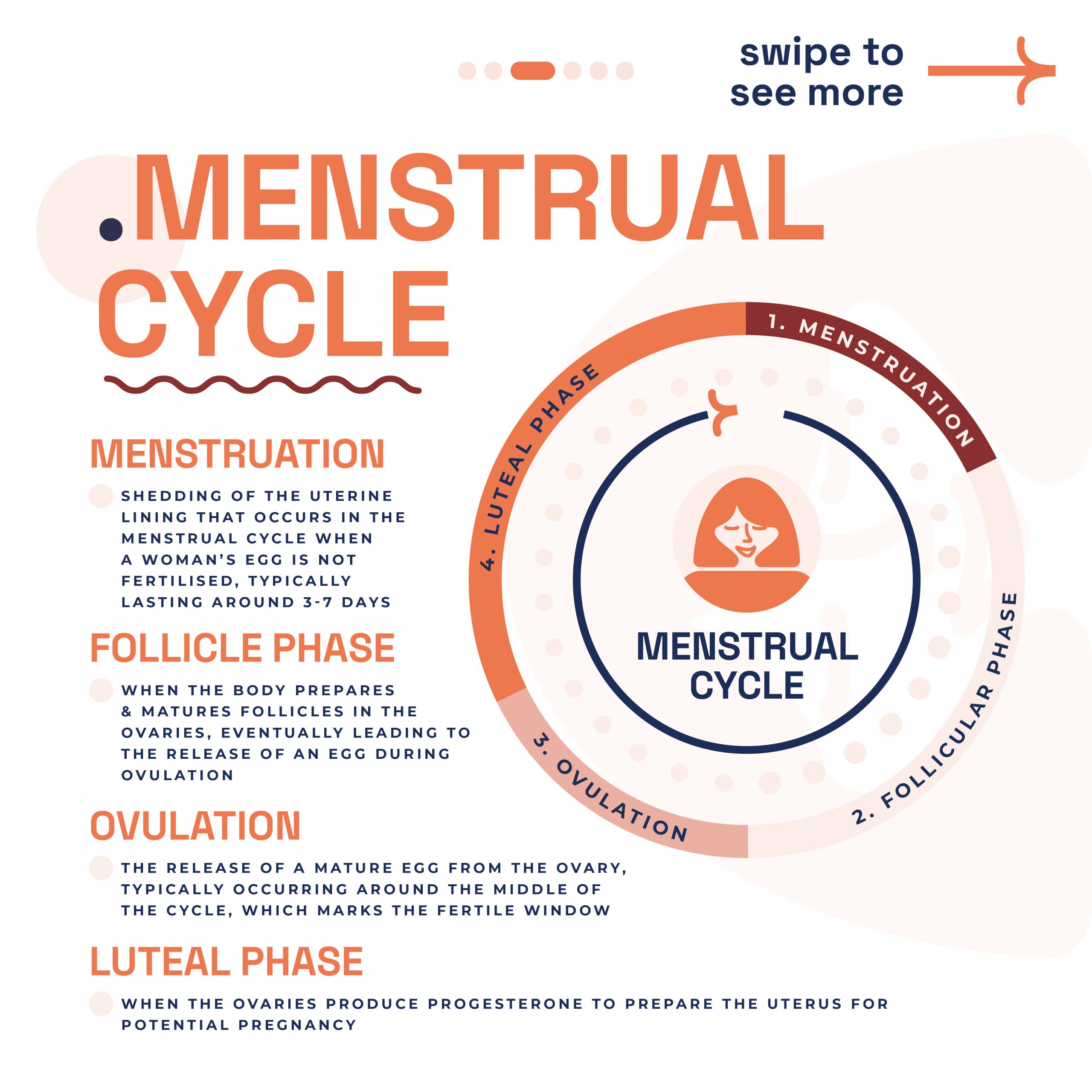
Fertility Scans: We specialise in fertility scans, including follicle tracking and endometrial lining scans. These scans monitor the growth and development of follicles, pinpoint ovulation, and enhance fertility treatment outcomes. Our endometrial lining scan evaluates the thickness and health of the endometrium, determining the best period for embryo implantation. These scans are crucial in both natural and assisted reproductive journeys.
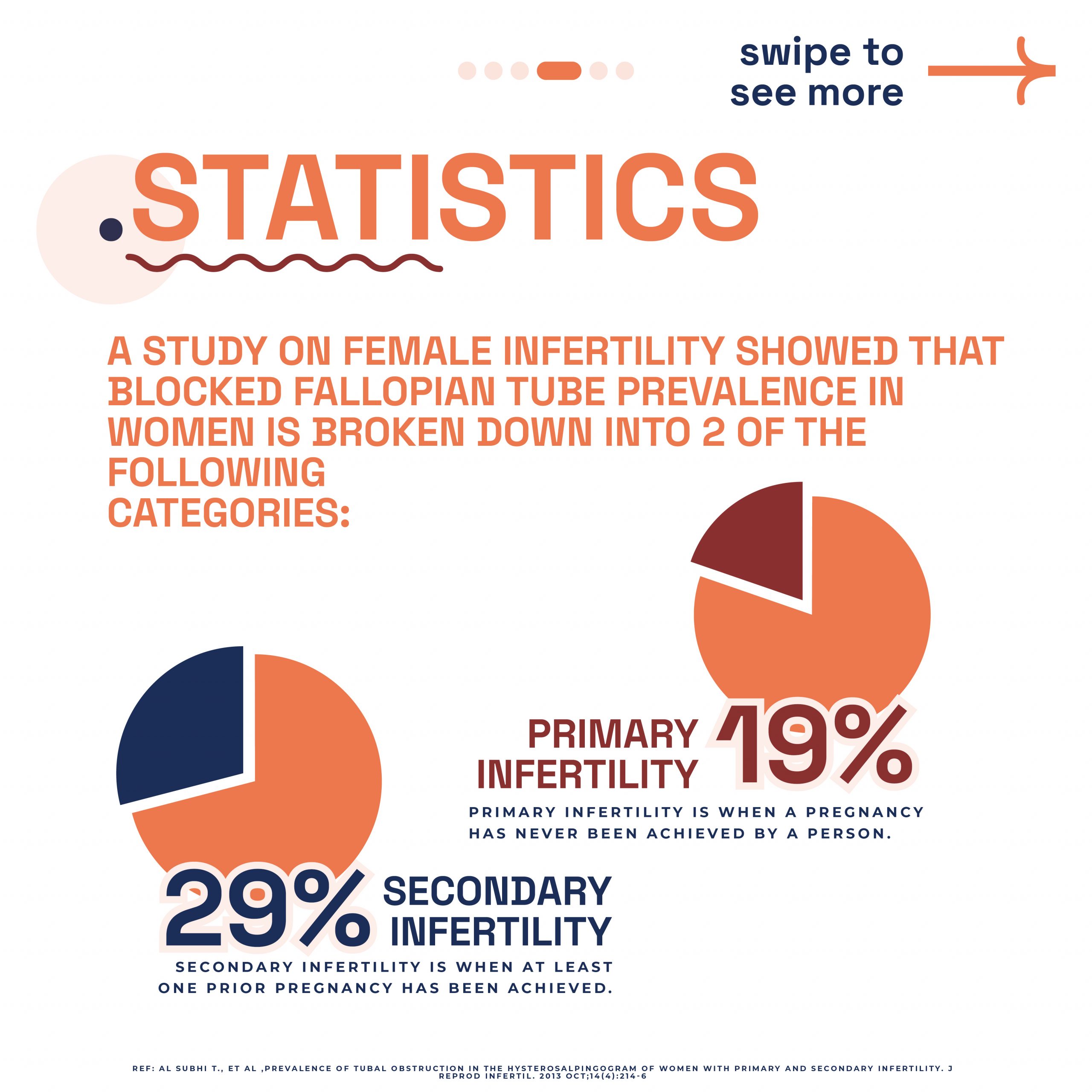
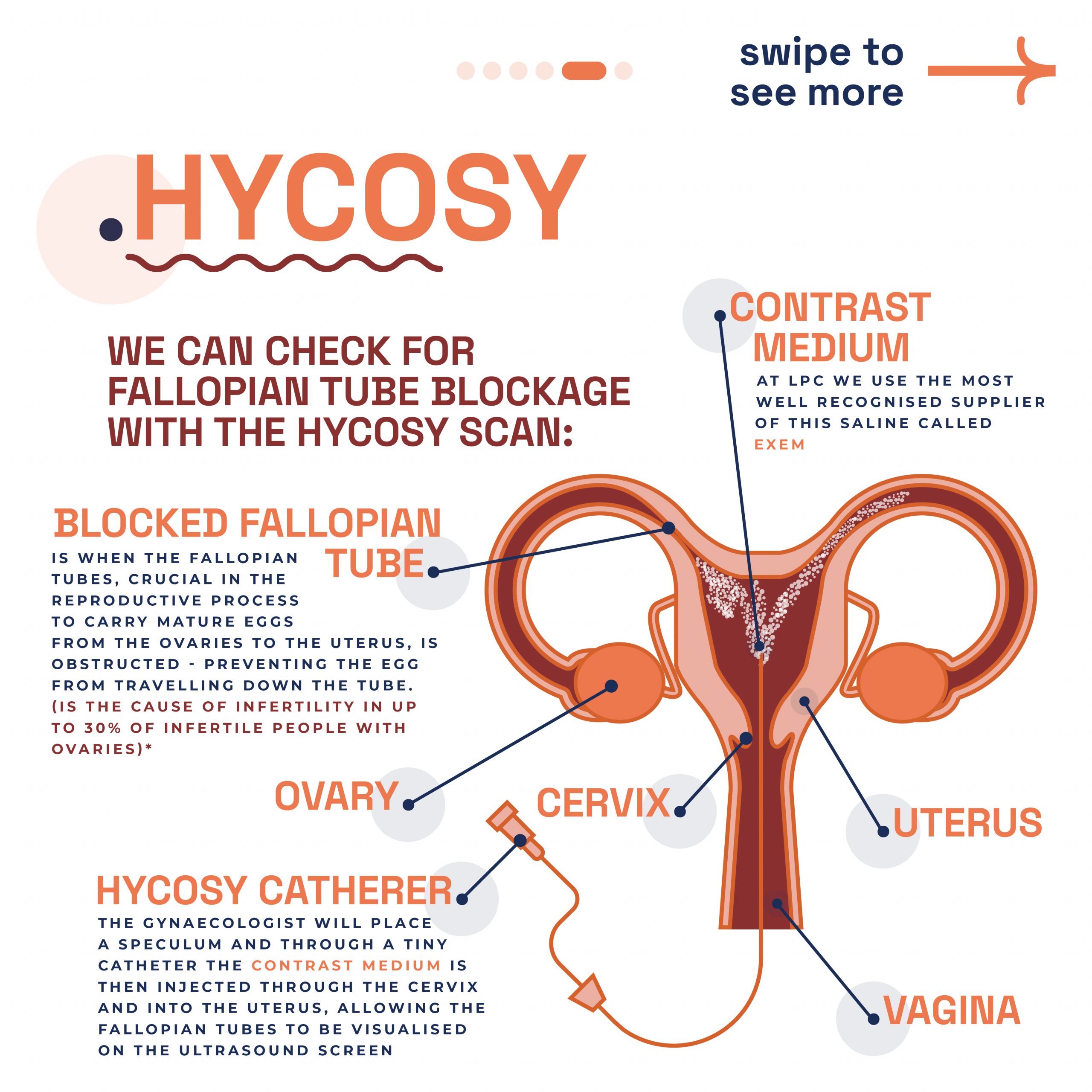
HyCoSy and 3D SIS Scans: We offer Hysterosalpingo Contrast Sonography HyCoSy and 3D SIS scans to examine the uterus and fallopian tubes. These non-invasive procedures provide detailed images to detect blockages or abnormalities, ensuring a thorough evaluation of your reproductive health.
Pregnancy
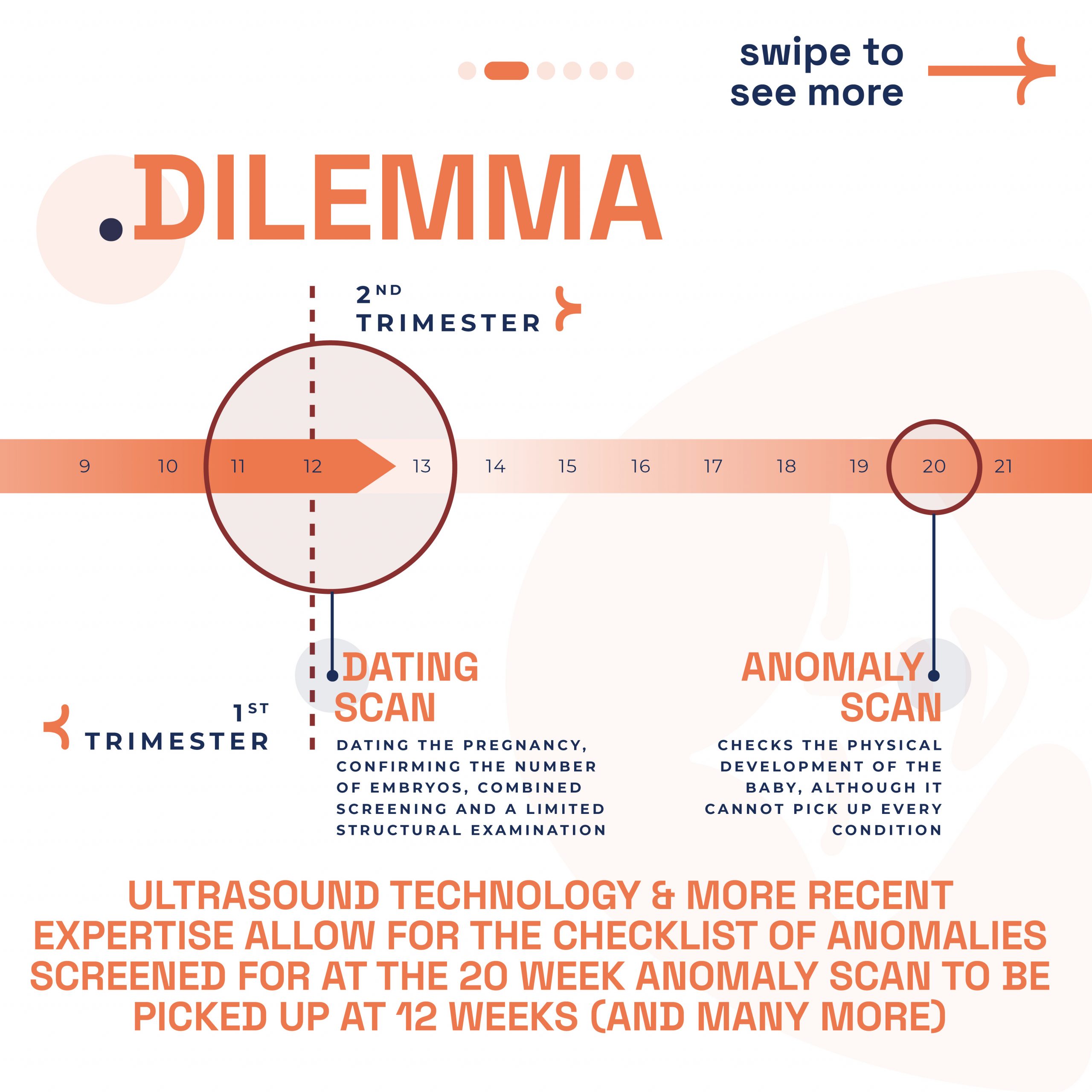
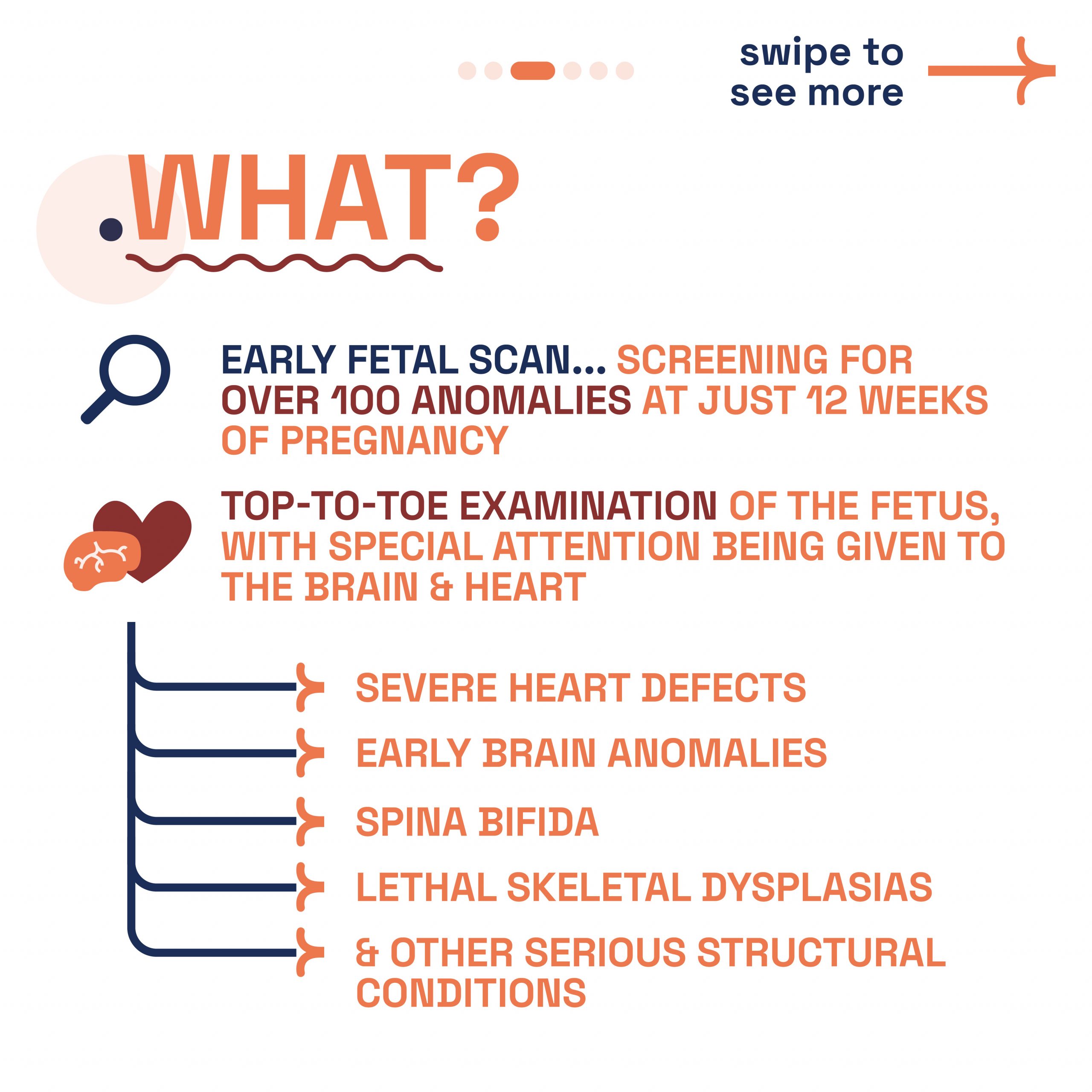
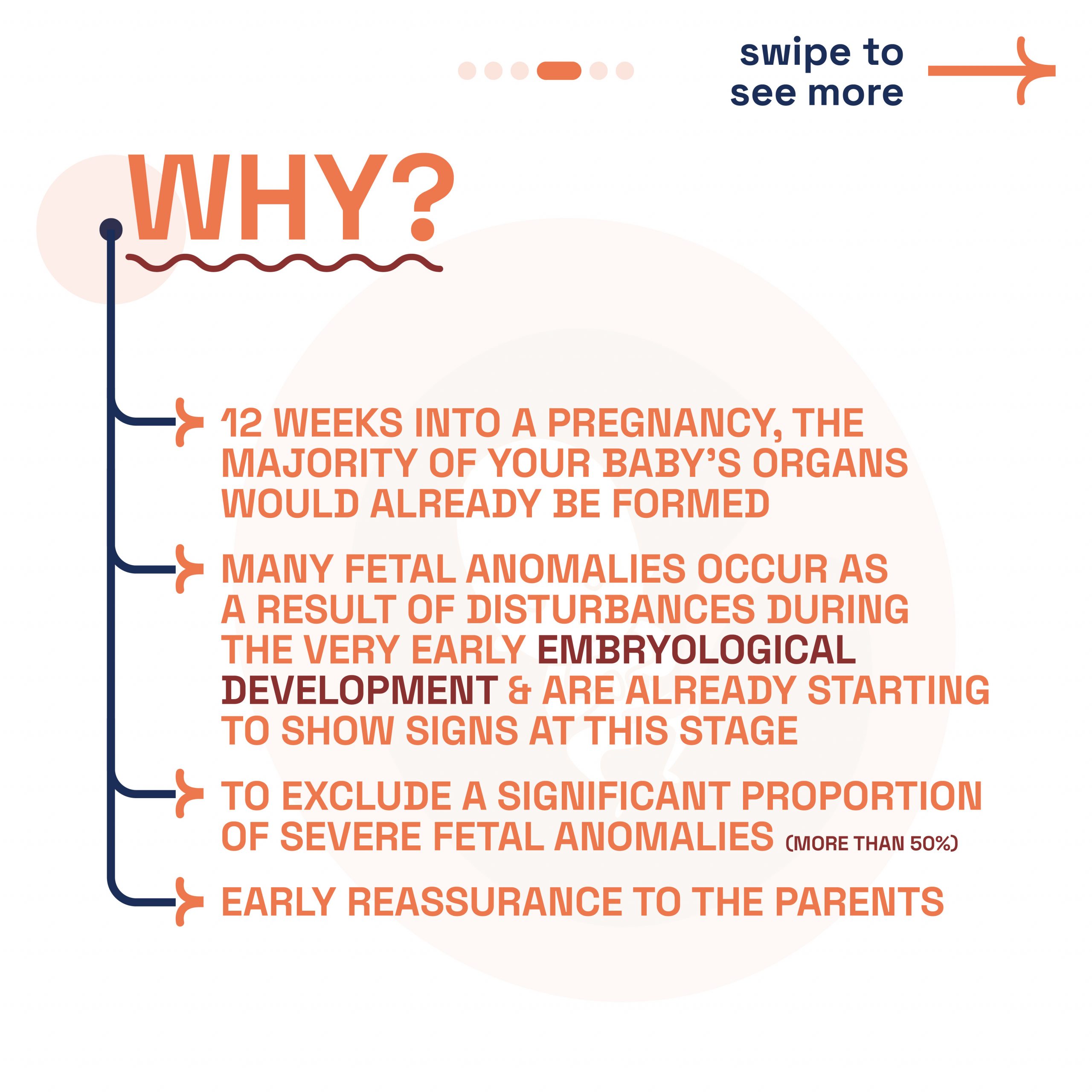
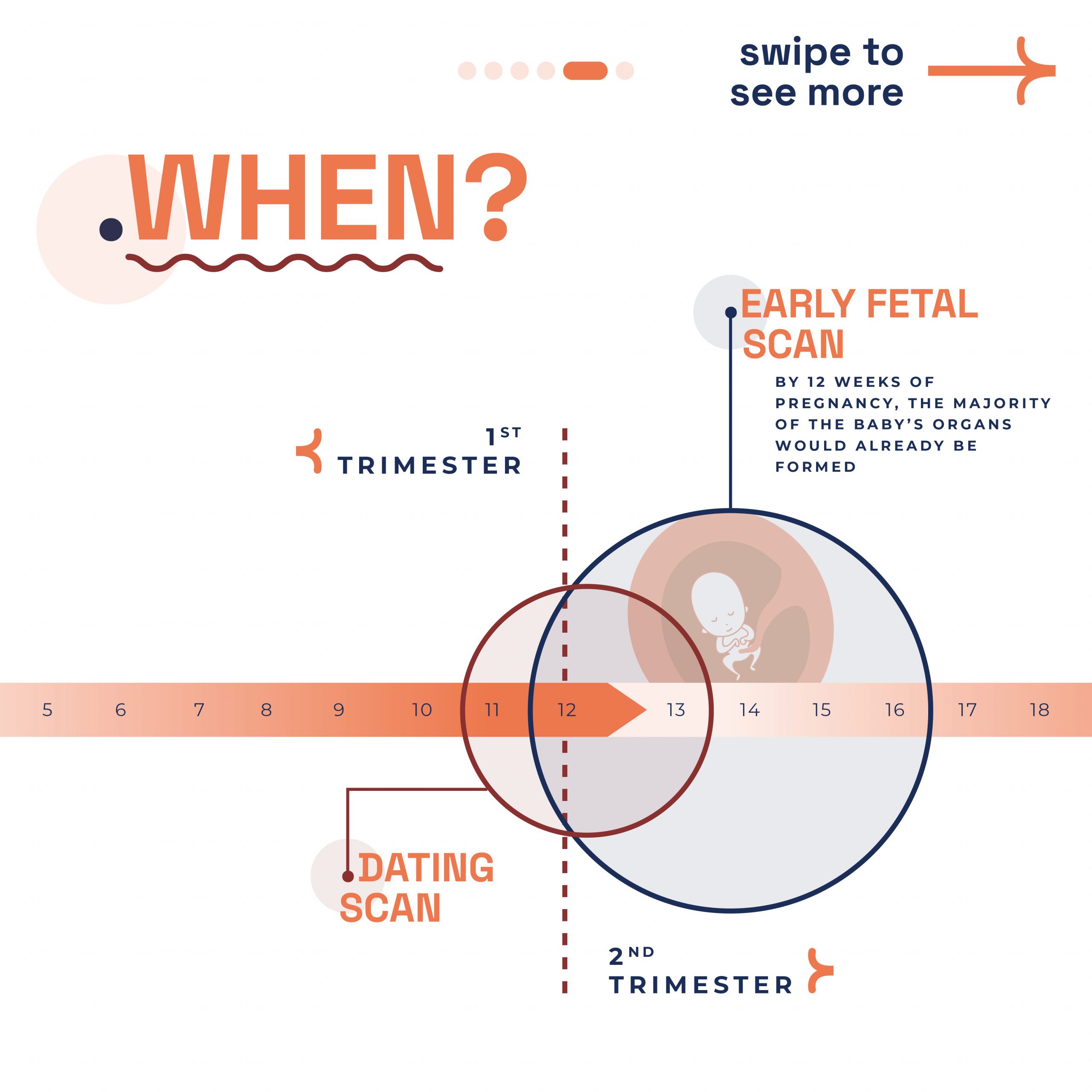
Pregnancy Ultrasound Scans: Our clinic provides a range of prenatal scans to monitor your baby’s health at every stage of pregnancy. We use the latest 2D, 3D, and 4D ultrasound imaging technology to offer clear and detailed insights. From viability scans at 6-9 weeks to anomaly scans in the third trimester, our comprehensive approach ensures you receive the best care.
Non-Invasive Prenatal Testing (NIPT): LPC is a leading provider of NIPT in London. This advanced screening option detects Down’s syndrome and other chromosomal conditions. NIPT can be performed from 10 weeks of pregnancy and is the most accurate, safest screening test available. Our SMART Test combines NIPT with ultrasound, providing a comprehensive screening for a range of rare diseases and anomalies.
Holistic Care: Our holistic approach includes support from conception to birth. We offer a welcoming and homey environment, ensuring you feel comfortable throughout your journey. Our team worked hard to design a space that was both inviting and informative. Attendees appreciated the effort, and our totes, filled with useful information, were a big success.
Thank You
Thank you to everyone who stopped by to chat with us. Your enthusiasm and dedication to advancing fertility and prenatal health are truly inspiring. We’re excited to keep these conversations going and continue supporting you on your journey to parenthood.
Final Thoughts
Participating in the Fertility Show 2024 was a significant milestone for LPC. We are dedicated to supporting individuals and couples on their fertility journey, providing expert care and guidance every step of the way. Stay tuned for more updates and connect with us for the latest in prenatal care and fertility support. If you missed us at the show or would like to learn more about our services, please contact us directly to schedule a consultation. Together, we can make your dream of parenthood a reality.