What is folic acid?
Folic acid is a synthetic (man-made) form of the Vitamin B-9 (folate), which naturally occurs in some foods such as asparagus, peas and broccoli. Folate supports generation of healthy new red blood cells, which carry oxygen around the body. The deficiency of red blood cells may be conditions like anaemia, which often causes weakness and fatigue.
Why is folic acid often recommended to women during their pregnancies?
Prior to conception and within the first trimester (around week 12) it is often recommended that women take this artificial supplement to reduce the risk of a neural tube defects and ensure the healthy formation of red blood cells. Taking folic acid Folic acid also supports maternal tissue growth and increases maternal folate to reduce risk of neural tube defect. Can reduce the risk of developing neural tube defects by up to 70% (WHO, 2015).
What is a neural tube defect?
The neural tube is an embryonic structure that lays the foundation for the central nervous system (consisting of the brain and spinal cord). Neural tube formation begins just three weeks after conception, and proper formation is vital for brain development. Neural tube defects occur when the formation of the neural tube does not develop or form correctly. These may result from a lack of folic acid in the first 28 days of pregnancy, causing the neural tube to poorly develop. Typically, the neural tube closes in the 4th week following conception. Neural tube defects include birth defects of the skull and brain like acrania or encephalocele, spine and spinal cord, such as spina bifida.
How much folic acid is recommended?
It is recommended that those who are planning to get pregnant take 400 micrograms supplement daily (NICE, 2014) both prior to pregnancy and for the first 12 weeks. The NICE recommend taking this supplement regardless of whether you are eating folate-rich foods.
Your GP may prescribe or recommend a higher dose if you have a BMI over 30, have diabetes, anaemia, sickle–cell disease, coeliac disease, take medication for epilepsy or have a history of neural tube defects.
What foods contain folic acid?
Asparagus, peas, broccoli, oranges, bananas. Green beans, kale, spinach, yeast extract and fortified cereals.
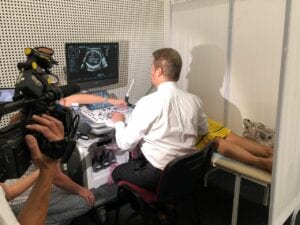
Can you detect neural tube defects by ultrasound?
Yes – Dr Ushakov has been developing new methods for detecting these anomalies in the first trimester from as early as 10 weeks.
For support for spina bifida and hydrocephaly: Shine Charity
Sources:
NICE (2014). Maternal and Child Nutrition [Online] [link]
NICE (2021). Neural Tube Defects (Prevention in Pregnancy) [Online] [link]
SHINE (2021). Folic Acid. [Online] [Link]
Ushakov, F., Sacco, A., Andreeva, E., Tudorache, S., Everett, T., David, A.L & Pandya, P. P. (2019). Crash Sign: New First‐Trimester Sonographic Marker of Spina Bifida. [Online] [Link]
World Health Organisation (2015). Prevention of Neural Tube Defects by The Fortification of Flour with Folic Acid: A Population-Based Retrospective Study in Brazil. [Online] [link]