Week 5 of Pregnancy

Week 5 of your Pregnancy
Discovering your baby’s progress since week 4
-
Published
-
Last Modified
Tags
Having journeyed through the early whispers of Week 4, we now step into the heart of your pregnancy story: Week 5. It’s a chapter filled with vibrant growth and transformation. Imagine your little one, still as tiny as an apple seed, beginning a significant journey into the embryonic period.
Week 5 of pregnancy, it’s all about growth and transformation. Your little one is busy developing, cell by cell, quickly growing from the size of a poppy seed in week 4 (watch video here) to an apple seed. We’ll explore these changes together, learn how to take care of yourself during this time and get a peek into your baby’s development with early ultrasounds. So, let’s dive into Week 5, where every day brings something new and amazing in your pregnancy journey. So let’s navigate the changes unfolding, how to care for yourself, and what to expect from medical check-ups.
Key Concepts: embryonic period
During Week 5 of your pregnancy, a crucial phase begins as your baby, the size of an apple seed, enters the embryonic period. This week marks the foundation for major organs and systems. Hormonal changes, especially increases in progesterone and human chorionic gonadotropin (hCG), are vital in supporting this stage. These hormones maintain the uterine lining and ensure the continuation of progesterone production, crucial for pregnancy health. As a result, you might notice early symptoms like fatigue and nausea. Understanding these changes is key to navigating the early stages of your pregnancy journey.
Pregnancy Checklist at 5 Weeks
While it’s still early in your pregnancy, there are some important steps you can take:
- Confirm your pregnancy with a test if you haven’t already.
- Schedule your first prenatal appointment to discuss your health and pregnancy. At London Pregnancy Clinic it’s called the Viability/Dating Scan. Use our pregnancy calculator to work out the best time for your scan.
- Begin focusing on a pregnancy-safe diet and lifestyle, emphasising foods rich in folic acid and essential nutrients.
Developmental Milestones: Week 5
Growth of the Gestational Sac: This week, the gestational sac, housing your developing baby, continues to grow. It’s a clear sign of your pregnancy’s progression, providing a protective and nourishing environment for the embryo.
Yolk Sac Development: The yolk sac plays a crucial role at this stage, providing essential nutrients before the placenta is fully operational. It also contributes to the early stages of the circulatory system by producing blood cells, supporting the developing embryo’s needs. This process is essential for supporting the growing needs of your embryo and is closely tied to the growth of the gestational sac.
Heart Development: Now your baby’s heart begins its incredible journey. Initially emerging as a simple tube-like structure, it’s preparing to pulsate and evolve into a sophisticated four-chambered heart in the coming weeks. Although it’s not beating just yet, this early stage sets the stage for one of life’s most vital rhythms.
Brain and Spinal Cord Formation: Alongside the heart, the neural tube, which will become the brain and spinal cord, starts to take shape. This tube forms the bedrock of the entire nervous system, integral for everything from physical movements to cognitive functions. It’s a complex process that lays the foundation for your baby’s future mental and physical capabilities.
Emergence of Other Organs: Week 5 also marks the beginning of other organ formations. Organs like the kidneys and liver start to form, albeit in their very preliminary stages much like the heart.
What is seen on the Ultrasound: Week 5?
During the Week 5 ultrasound, expect to see the gestational sac (which has dramatically increased in size since Week 4), the first structure visible on an ultrasound, indicating your pregnancy is progressing well. This small, fluid-filled sac is where your baby will develop. Inside it, the yolk sac may also be visible, which is crucial for providing nutrients to the developing embryo and for blood cell production in these early stages. However, it’s important to remember that at this stage, the embryo itself and its heartbeat are usually not yet detectable.
It’s common not to see the embryo or hear a heartbeat during a Week 5 ultrasound. The embryo is still very small, and the heartbeat typically becomes detectable around the 6th or 7th week of pregnancy. While we know it’s tempting to have an early ultrasound, we at London Pregnancy Clinic recommend waiting until at least week 6 for your first scan. This crucial ultrasound provides a tangible glimpse into your pregnancy, offering reassurance and joy as you embark on this extraordinary journey.
-

Gestational sac at 4 weeks of pregnancy as seen on ultrasound scan.
-
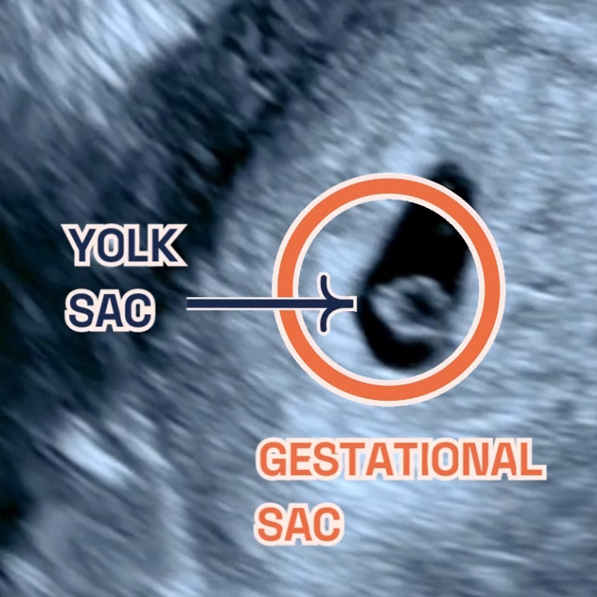
Gestational sac and yolk sac at 5 weeks of pregnancy as seen on ultrasound scan.
Thinking ahead: Week 6?
Looking forward to Week 6, expect continued development of your baby’s facial features. You may also start experiencing more pronounced pregnancy symptoms like nausea and fatigue. It’s a time to start preparing both mentally and physically for these changes.
Week 5 of Pregnancy FAQs
-
How common is it for my baby to have a heartbeat at 5 weeks?
Your baby is an embryo (not a fetus just yet) and can have a heartbeat at 5 weeks of pregnancy, but it is not very common. The fetal heartbeat usually starts to beat between 5 and 6 weeks gestation, and it may be detectable via ultrasound around this time.
Here are some reasons why the heartbeat might not be detected on an ultrasound at 5 weeks:
- The embryo is too small.
- The heartbeat is too faint.
-
What if there is no yolk sac at 5 weeks?
Patients have asked us why is there no sac seen when 5 weeks pregnant. The yolk sac is usually visible on an ultrasound between 5 and 6 weeks gestation. If there is no yolk sac visible on an ultrasound at 5 weeks, it could be a sign of a miscarriage.
However, it could be a sign that the estimated gestational age is wrong. This could happen if your last menstrual period was inaccurate or if you were ovulating later than you thought.
In this case, we may recommend a follow-up ultrasound in a week or two to see if the yolk sac has developed.
Conclusion
Week 5 of your pregnancy is a time of rapid and incredible changes. While you might start feeling different physically and emotionally, remember, these are signs of your baby’s healthy development. Stay informed, take care of yourself, and prepare for the exciting journey ahead. If you have any concerns, our team at London Pregnancy Clinic is always here to guide you.
Stay tuned on what your baby’s week-by-week growth will look like on our blog.