Blood Tests During Pregnancy

Blood Tests During Pregnancy:
Ensuring the Health of You and Your Baby.
-
Published
-
Last Modified
Tags
At London Pregnancy Clinic, we understand the importance of precise blood tests for monitoring health and diagnosing conditions during pregnancy. Explore the essential tests that help ensure the well-being of both mother and child.
While blood tests during pregnancy aren’t essential, they can significantly enhance your preparedness. Your healthcare provider may recommend a tailored series to monitor your health and your baby’s growth. These tests are invaluable for early detection of potential health issues, enabling prompt and effective interventions. At London Pregnancy we offer a wide variety of tests, which in this blog, we will dive into.
Why Consider Blood Tests During Pregnancy?
Blood tests during pregnancy offer invaluable insights into both maternal and fetal health, enabling better preparedness and care. Here are several compelling reasons to consider these tests:
Monitor Maternal Health: Blood tests, such as the complete blood count (CBC) and liver function tests, assess the mother’s overall health. They check for conditions like anaemia, infections, and gestational diabetes that may require close monitoring or specific treatments.
Assess Fetal Health and Development: Genetic screening tests can detect chromosomal conditions such as Down syndrome, Edwards syndrome, and Patau syndrome. These tests, often paired with ultrasounds, help evaluate the risk of certain genetic disorders, guiding further prenatal care. We offer Non-Invasive Prenatal Testing (NIPT) from 10 weeks of pregnancy and can help you choose the right NIPT for you!
Identify Rh Incompatibility: Determining the mother’s blood type and Rh factor is crucial. Rh incompatibility can lead to serious complications, necessitating special treatment to safeguard the baby’s health. At LPC we currently don’t offer Rh factor blood test (at the time of writing April 2024). However, during your NHS antenatal checks you will be able to get it. Read more on Rhesus Disease RhD on the NHS website.
Screening for Infectious Diseases: Screening for infectious diseases like hepatitis B, HIV, and syphilis is critical. Identifying these infections early allows for steps to be taken to prevent transmission to the baby, ensuring a safer delivery.
Provide Baseline Information: The results from initial blood tests create a baseline that helps monitor the pregnancy’s progression. Any significant changes can be quickly identified, allowing for timely interventions.
Overall, considering blood tests during pregnancy is vital for early detection of potential issues. These tests enable timely and effective interventions, ensuring the health and wellbeing of both mother and baby.
Why Consider Blood Tests for Pregnancy Confirmation?
Pregnancy tests, including urine and blood tests, are designed to confirm if you are pregnant. Urine tests are widely used due to their convenience and availability over-the-counter. However, blood tests, particularly the Beta HCG (Human Chorionic Gonadotropin) test, provide more comprehensive insights.
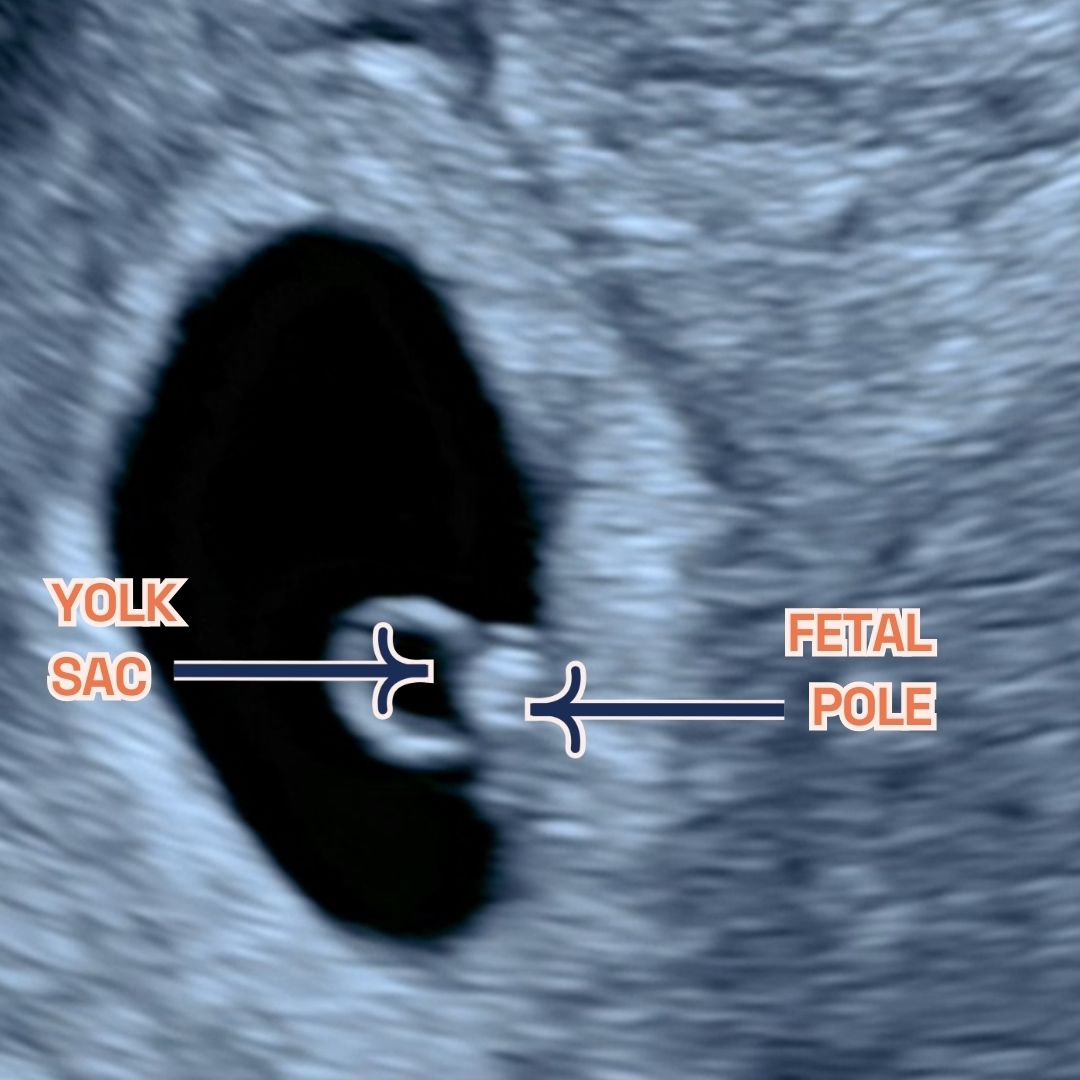
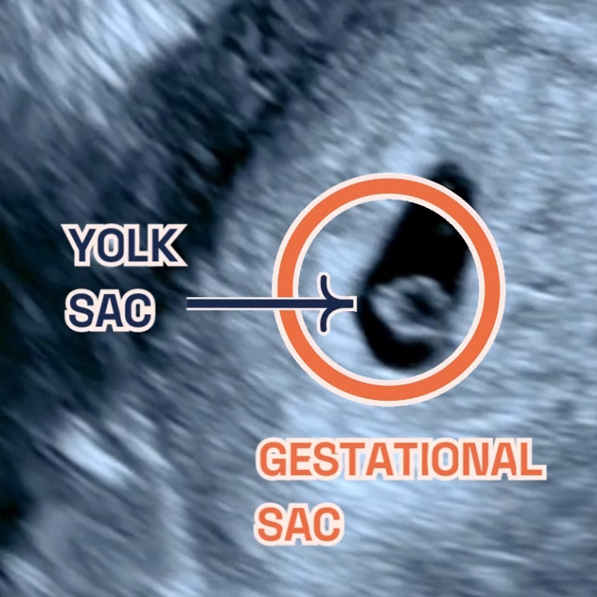
The Beta HCG test detects the hormone produced by the placenta shortly after implantation, appearing in the blood about 11 days post-conception, which is slightly earlier than in urine. It is essential for confirming early pregnancy and is available in two types: the Qualitative HCG Test, which simply indicates pregnancy with a ‘yes’ or ‘no’, and the Quantitative HCG Test, which measures exact HCG levels in the blood for high accuracy.
Unlike urine tests, the Beta HCG test requires a blood sample taken in a healthcare setting and is more sensitive, offering early detection and additional information such as the approximate age of the fetus and potential complications. This makes blood tests a vital tool for early and accurate pregnancy confirmation.
What is the AMH Blood Test?
The AMH blood test measures the levels of AMH in a woman’s blood, a hormone produced by ovarian follicles. It serves as a reliable marker of ovarian reserve, indicating a woman’s potential fertility. This test is instrumental for clinicians and fertility specialists to predict a woman’s response to fertility treatments, like in vitro fertilisation (IVF).
AMH levels provide a reliable measure of a woman’s ovarian reserve, although they do not directly correlate with egg quality. Low AMH levels might suggest a diminished ovarian reserve, posing concerns for natural conception or IVF. Conversely, high AMH levels might indicate conditions like Polycystic Ovary Syndrome (PCOS).
AMH testing is crucial in assisted reproductive technology, aiding in the development of personalised IVF treatment strategies. Women with low AMH may respond less to ovarian stimulation, affecting egg retrieval numbers and IVF success rates. High AMH levels can increase the risk of Ovarian Hyperstimulation Syndrome (OHSS), especially under strong fertility medication effects.
Preparing for Your Blood Test
Our blood tests at London Pregnancy Clinic are perfect for accurately confirming pregnancy, monitoring early viability, and following up post-IVF. We offer convenient same-day appointments that fit your schedule. To ensure accurate results, follow the specific instructions provided by your healthcare professional. These may include:
- Fasting Requirements: You might need to avoid all food and drinks, except water, for up to 12 hours before certain tests.
- Medication Guidelines: It may be necessary to pause specific medications temporarily. This will prevent any interference with your test results.
Adhering to these guidelines is crucial. Incorrect preparation can affect your results, possibly requiring a repeat of the test. Check-in with your care provider about what you should do! At London Pregnancy Clinic you can call our reception and our team will gladly help with any queries!
Please note, that these tests require a referral from an existing provider. We will send the results to both you and your nominated healthcare provider upon request.
Get to Know Your Phlebotomist
Molly, one of our skilled phlebotomists, ensures that your blood tests are conducted smoothly, providing a comforting presence during the process.
Final Thoughts
The results from these tests provide a snapshot of your health and that of your baby, allowing your healthcare provider to tailor your prenatal care effectively. Remember, it’s crucial to discuss any concerns with your healthcare provider.
Our selection of blood tests is available exclusively to patients holding a referral from their healthcare provider, ensuring you receive the highest standard of care. We send samples to a partnered laboratory for precise analysis. If you need a referral or interpretation of blood test results, our friendly reception team is ready to help you book an appointment with the appropriate consultant. Please remember, if you’re coming for a pregnancy scan, our sonographer cannot refer you for a blood test. Referrals for blood tests are only possible through an appointment with our Consultant Obstetricians or Gynaecologists. At the LPC, we’re here to support you from the very first step.
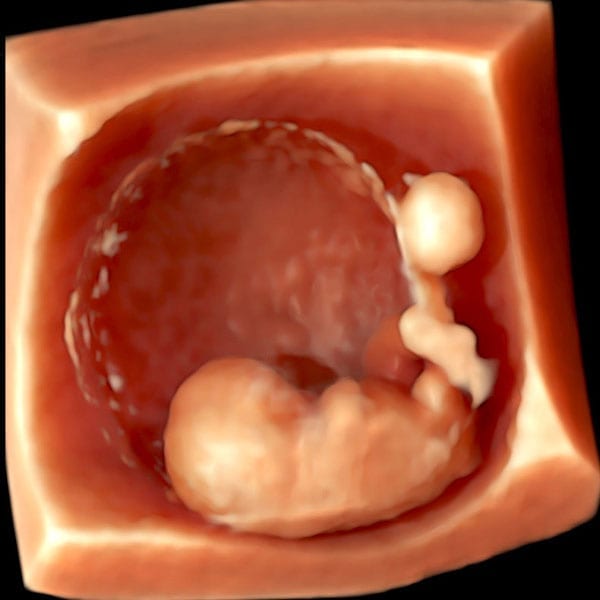
Want to book a blood test with us? Visit our Blood Tests page or give us a call! If you already had your pregnancy confirmed, we recommend booking an early pregnancy scan to check for the baby’s development.