What is a Doula?

What is a Doula?
Celebrating the World Doula Week by shedding light on what they do.
-
Published
-
Last Modified
Tags
Celebrate World Doula Week with us and discover what is a Doula and the invaluable support they offer to expectant mothers. From emotional support to physical and informational assistance during childbirth, doulas play a crucial role in enhancing the pregnancy experience. Learn how a doula can be part of your journey to motherhood, providing reassurance and strength every step of the way.
As we welcome World Doula Week, let’s spotlight the pivotal role of doulas in the childbirth journey. A doula, known for offering profound support, stands by individuals through childbirth, miscarriage, induced abortion, and stillbirth. Their role transcends mere presence, embracing emotional, physical, and informational support. Doulas guide expectant parents, turning the childbirth process into a more informed, empowering experience.
They shine as beacons of knowledge and comfort, ensuring parents feel heard, valued, and respected. By offering a hand to hold, an ear to listen, and a wealth of knowledge, doulas make the path to parenthood less daunting. Their support is not just about the birth process but about fostering a positive, empowering environment for all involved. Doulas help navigate the complex emotions and decisions that come with childbirth and beyond.
What is a Doula?
The term “doula” has its origins deeply rooted in the ancient Greek word δούλα, meaning “a woman who serves”. Over centuries, this concept has significantly evolved, especially during the grassroots natural birth movement in the United States in the 1960s. This era marked a pivotal shift, as women started advocating for unmedicated, low-intervention births, bringing to light the desire for supportive companionship during childbirth that went beyond medical assistance.
Originally, the concept of a doula focused on emotional and physical support during labour and delivery. However, their role has expanded, embodying a comprehensive support system for various stages of pregnancy, including preconception, miscarriage, and postpartum periods. Doulas are now pivotal figures in the childbirth journey, offering guidance, comfort, and advocacy.
Doulas stand out for their personalised care approach. They tailor their support to meet each family’s unique needs, ensuring a more positive and informed pregnancy and birthing experience. From helping devise birth plans to offering strategies for pain management, doulas empower parents-to-be with knowledge and confidence.
Today’s doulas embody this rich heritage, offering non-medical, emotional, and practical support to families during one of the most transformative periods of their lives (this is what sets them apart from midwives). They draw on formal and practical knowledge to empower expectant mothers to have the birth experience they desire, whether it be at home, in a birthing centre, or in a hospital setting. The evolution of the doula’s role from a grassroots movement to a recognised profession underscores a growing appreciation for personalised care and the profound impact of dedicated support during pregnancy, childbirth, and the postpartum period.
The Role of a Doula
Doulas offer a holistic support system that addresses the emotional, physical, and informational needs of expectant families. Their comprehensive care ensures that mothers feel cherished, bodies are respected, and decisions are well-informed, paving the way for a positive and empowered birth experience.
Emotional Support: Doulas provide unparalleled emotional backing, blending compassion with encouragement. Their role goes beyond mere presence; they become confidants to expectant mothers, offering a listening ear during moments of doubt and joy alike. This emotional scaffolding ensures mothers navigate their pregnancy journey feeling thoroughly supported and deeply understood. The reassurance doulas offer becomes a pillar of strength, fostering a sense of calm and confidence as birth approaches.
Physical Support: In the realm of physical comfort, doulas excel with their hands-on approach. Employing techniques such as massage and recommending various birthing positions, they significantly ease the physical strains of labour. Their expertise in comfort measures transforms the birth experience, making pain more manageable and labour more bearable. By intuitively responding to a mother’s needs, doulas facilitate a smoother birthing process, where discomfort is alleviated, and mothers feel more in control of their bodies.
Informational Support: Armed with evidence-based insights, doulas are invaluable guides through the maze of childbirth and postpartum care. They demystify medical procedures and explain care options, empowering families to make choices that resonate with their values and desires. This informed support ensures that decisions around birth and aftercare are made with clarity and confidence. Doulas’ dedication to providing accurate, up-to-date information helps families approach childbirth with informed optimism, prepared for the journey that lies ahead.
Types of Doulas
Birth Doula: Birth doulas can play a crucial role in supporting expectant mothers through pregnancy, labour, and childbirth. They offer continuous emotional support, guidance, and reassurance. These professionals work closely with families, preparing them for the birthing process, assisting in creating birth plans, and providing techniques for pain management. Their presence ensures a comforting and empowering experience, helping mothers navigate the challenges of childbirth with confidence and calm.
Postpartum Doula: In the early days following a baby’s arrival, postpartum doulas become an invaluable source of support for new families. They assist with newborn care, offer breastfeeding support, and help manage household tasks, allowing parents to focus on bonding with their baby. Their knowledge and experience in postpartum care provide a smooth transition for families during this new chapter, ensuring both the baby’s and the mother’s needs are met with compassion and expertise.
Fertility Doula: Fertility doulas offer support to families facing challenges in conceiving. They provide emotional backing, resources, and guidance through fertility treatments and decisions. By offering a listening ear and informed advice, fertility doulas help couples navigate the often complex and emotional journey towards conception. Their role is to empower and support families, ensuring they feel understood and supported every step of the way.
Each type of doula specialises in catering to the unique needs of families during different stages of the pregnancy journey. Their dedicated support ensures that expectant and new parents feel empowered, informed, and cared for, making the journey to parenthood a more positive and fulfilling experience.
Benefits of Having a Doula
Having a doula during childbirth brings numerous advantages. Notably, mothers with doulas often experience reduced intervention rates, such as fewer cesarean sections and less need for pain relief medication. This support can lead to shorter labour durations, allowing mothers to recover more swiftly post-birth. The presence of a doula often results in more positive birth experiences, with mothers feeling empowered and satisfied with their childbirth journey. Crucially, the enhanced emotional support provided by doulas strengthens the overall well-being of mothers and families, creating a nurturing environment for welcoming new life.
How to Choose a Doula
Selecting the right doula is pivotal for a supportive childbirth experience. Begin by considering their training and experience; a well-trained doula can significantly impact your birth experience. Explore their philosophy on labour and childbirth to ensure it aligns with your personal preferences and values. Compatibility is key—your doula should feel like a natural extension of your support system. Seek recommendations from others who have had positive experiences with doulas. This can offer invaluable insights into potential matches. Finally, trust your instincts; the right doula should make you feel comfortable, heard, and respected.
Choosing a doula is a deeply personal decision, influenced by your unique needs and childbirth aspirations. By carefully considering these aspects, you can select a doula who will enhance your birthing experience, offering the support, knowledge, and care you deserve during this transformative time.
How are Doulas involved
Incorporating a fertility doula into the journey of fertility screening adds a deeply valuable layer of emotional guidance and support. They stand by individuals through the whirlwind of emotions that fertility testing can provoke, offering a comforting presence alongside medical treatments. This support extends to providing a safe, nonjudgmental space where individuals can freely express their concerns and uncertainties.
Fertility doulas excel in demystifying the processes involved in fertility screening. They educate on various fertility options and tackle mental blocks or anxieties that may surface. Their holistic approach aims not just to inform but to empower individuals, ensuring they approach each step with confidence and a well-understood perspective.
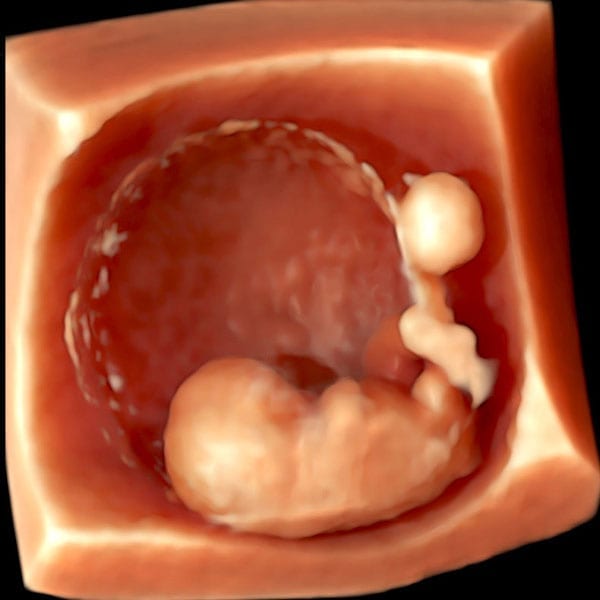
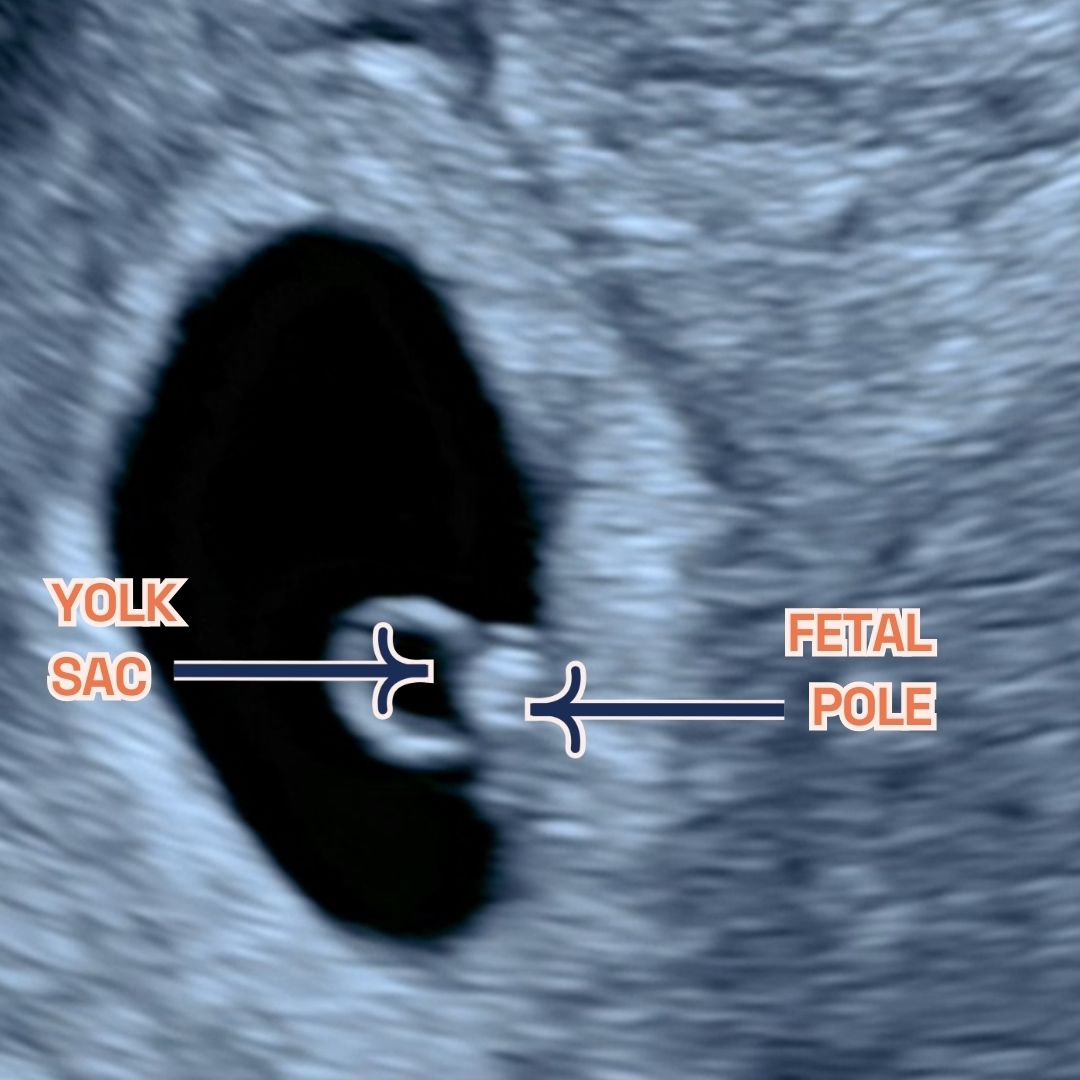
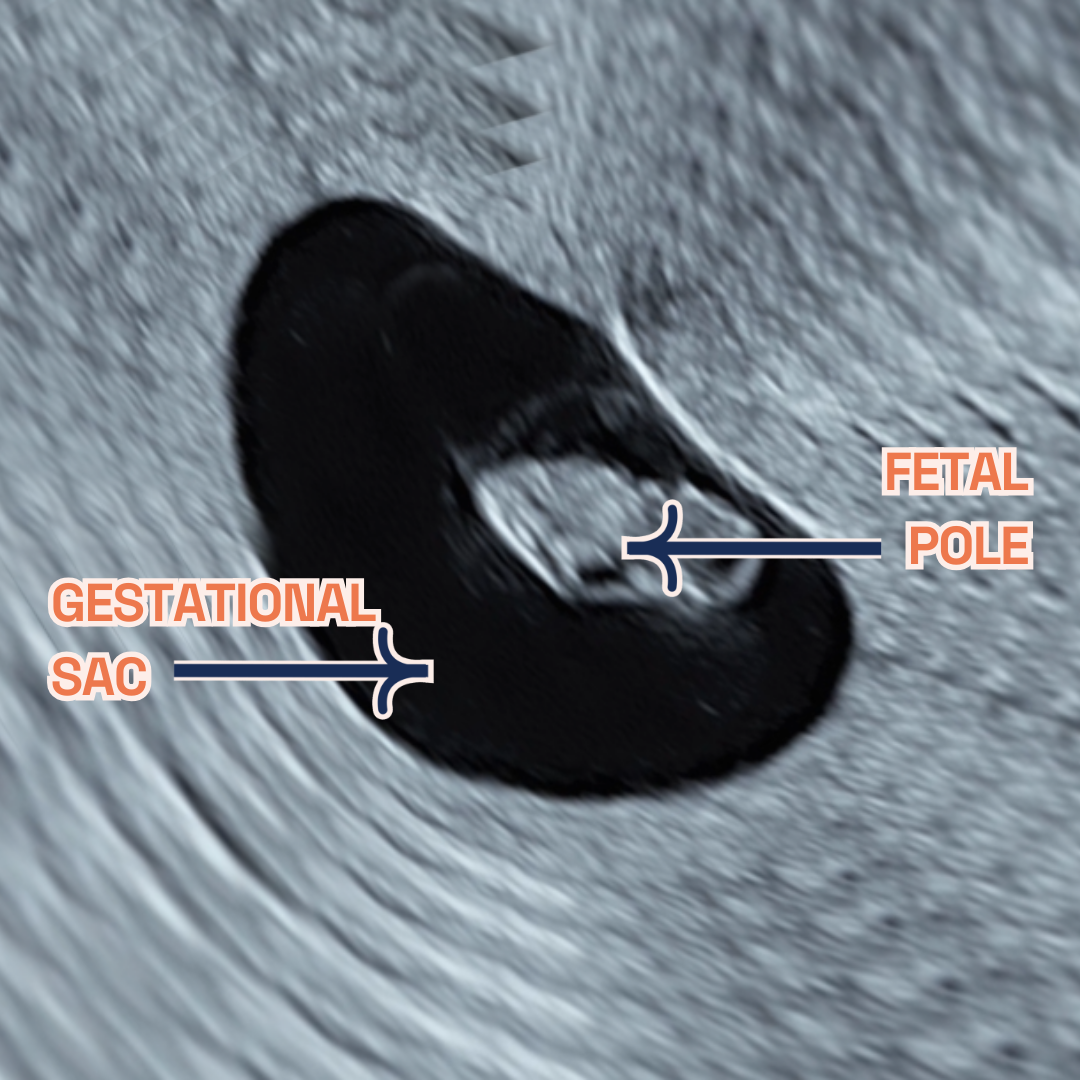
During ultrasounds, the role of a fertility doula becomes even more pronounced. Their emotional reassurance and ability to answer questions make a significant difference. They strive to create a serene, supportive environment, simplifying the ultrasound process and bolstering the individual’s spirits throughout the appointment. The calming influence of a doula can effectively mitigate any anxiety or apprehensions, significantly enhancing the overall ultrasound experience.
Fertility doulas provide more than just support; they bring clarity, confidence, and a sense of calm to the often complex and emotional journey of fertility screening. Their involvement ensures that individuals feel not only supported but also empowered and informed every step of the way.
Final Thoughts
You’ve discovered the crucial role of doulas in childbirth, providing emotional, physical, and informational support. Their support enhances the well-being of mothers, newborns, and families during pregnancy, labour, childbirth, and beyond, leading to empowering birth experiences.
Initiated by Ruti Karni Horowitz in Israel in 2011, World Doula Week starts on March 22, celebrating World Doula Day, and continues until March 28 every year. CAPPA’s enthusiastic backing helped turn Horowitz’s idea into a global celebration that welcomes all doulas and doula organisations.
This celebration highlights the positive impact of doulas: fewer C-sections, greater confidence in newborn care, shorter labours, fewer epidural requests, higher breastfeeding success, and increased satisfaction with the birth process. Doulas also play a role in reducing postpartum mood disorders. Chosen for its cultural significance of renewed fertility, March 22 aligns with the spring equinox, reflecting the doula’s role in welcoming and nurturing new beginnings worldwide.