Private NIPT Cost in London UK

Non-Invasive Prenatal Testing (NIPT) Cost in London
Published
Tags
NIPT, or Non-Invasive Prenatal Testing, is currently the safest and most accurate way to screen for chromosomal anomalies before your baby is born. However, NIPT cannot detect any physical or structural anomalies, which represent almost 2/3 of the fetal anomalies. That’s why we recommend doing NIPT with an early anomaly ultrasound scan from £490.
Short history of NIPT
- NIPT was first introduced in 2011 by Sequenom, using next-generation sequencing to analyze cell-free fetal DNA in maternal blood. This allowed screening for trisomies 21, 18 and 13.
- In 2012, Ariosa Diagnostics (now Roche) launched the Harmony test, also using cfDNA analysis. Natera’s Panorama test entered the market shortly after.
- These first-generation tests analyzed chromosomes 21, 18 and 13. Around 2013, companies began expanding NIPT to screen for sex chromosome aneuploidies.
- By 2016, Illumina had acquired Verinata, making them a major NIPT provider. Labs like Natera, Illumina, Roche and BGI continued enhancing their tests.
- In 2019, Illumnia launched the VeriSeq NIPT Solution v2 which added screening for microdeletions. Other labs followed with expanded NIPT panels.
- Currently, the major players providing NIPT globally are BillionToOne Unity, EuroFins PrenatalSAFE, Illumina, Natera, Roche/Ariosa, BGI, Yourgene Health, and PerkinElmer’s Labcorp. Some operate as test manufacturers while others partner with labs.
- NIPT technology and capabilities continue to advance rapidly. It is now recommended by many professional societies as a first-tier prenatal screening test due to higher accuracy than traditional serum screening. Adoption continues rising globally.

The importance of Ultrasound screening
There are a few key reasons why it is important to have an ultrasound scan in conjunction with NIPT:
- NIPT is a screening test, not a diagnostic test. Ultrasound helps confirm or identify potential fetal anomalies through visual imaging rather than just a probability result.
- Ultrasound provides important information that NIPT does not, including confirming gestational age, fetal presentation, number of fetuses, placental location, anatomical structures, and growth measurements.
- Soft markers for aneuploidy like increased nuchal translucency, absent nasal bone, echogenic bowel or cardiac anomalies may be detected on ultrasound but not by NIPT.
- If ultrasound dates do not match LMP dating, it can affect the accuracy of NIPT results. Ultrasound provides more precise gestational age.
- Ultrasound helps determine if discordant NIPT results may be due to placental, vanishing twin or maternal malignancy issues.
- Some structural defects like neural tube defects are not screened for by standard NIPT panels but may be visible on ultrasound.
- Ultrasound provides live visualisation of the fetus, which can help make NIPT results feel more real for parents.
While NIPT is an invaluable screening tool, ultrasound adds important clinical information and imaging. Following up abnormal NIPT results with ultrasound helps determine next steps for diagnosis and pregnancy management.

What is currently offered by the NHS?
The NHS Fetal Anomaly Screening Programme screens for the following anomalies:
- Down’s syndrome (trisomy 21)
- Edwards’ syndrome (trisomy 18)
- Patau’s syndrome (trisomy 13)
- Anencephaly
- Congenital heart defects
- Cleft lip
- Exomphalos
- Gastroschisis
- Spina bifida
- Serious musculoskeletal problems (such as limb reduction defects)
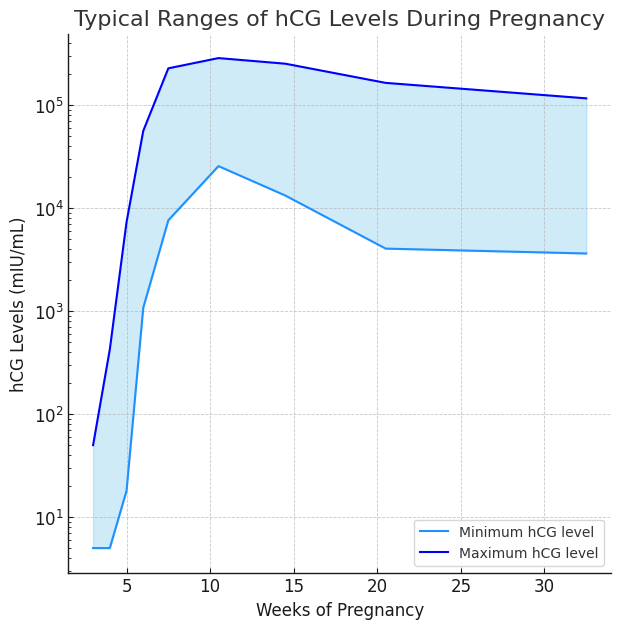
The screening is offered to all pregnant women between 10-14 weeks of pregnancy. It involves a blood test to measure two pregnancy hormones in the mother’s blood along with an ultrasound scan (nuchal translucency scan).
The screening provides a risk assessment as to the likelihood of the baby having one of the conditions, but it is not a diagnostic test. Those with a high-risk result are offered further tests such as amniocentesis or chorionic villus sampling to confirm a diagnosis.
The NHS screening programme aims to identify potential problems early in pregnancy so parents can make informed choices and access appropriate antenatal care and treatment if needed.