Week 7 of Pregnancy

Week 7 of your Pregnancy
Discovering your baby’s progress since week 6
-
Published
-
Last Modified
Tags
Embark on the transformative journey from Week 6 to Week 7 of your pregnancy with London Pregnancy Clinic. Experience the wonder of your baby’s growth with our private early pregnancy scans. Week 7 brings rapid development, from distinct heartbeats to the formation of facial features. Embrace the new changes and the reassurance of seeing your baby’s progress.
Stepping into Week 7 of your pregnancy, you’re embarking on a remarkable phase. Your baby, swiftly growing and developing, is now ready for the next stage of prenatal monitoring. At London Pregnancy Clinic, we understand the excitement and curiosity that comes with this week. It’s a time when many expectant mothers like Sarah and Emily seek reassurance through our private early pregnancy scans.
Key Concepts: fetal development
Baby’s Fast Heart Beat: During week 7, your baby’s heart rate accelerates, typically beating between 120 and 160 times per minute. This rapid heartbeat is a healthy sign of your baby’s growth and development. It’s an exhilarating moment for many parents, often heard for the first time during a viability scan.
Facial Features: By Week 7, your baby, roughly the size of a blueberry, shows significant development. The viability scan often reveals more distinct features and movements. The embryo’s facial features start taking shape, with the brain developing at a remarkable pace.
Rapid Development: 7 weeks marks the start of a huge growth spurt. During this period (between 7 and 20 weeks) your baby’s body parts will grow rapidly and organs such as the heart and brain will develop and increase in complexity. The basic structures of all major body parts and organs are formed during this time, with much of the growth being focused on the brain. Your baby’s brain cells are being generated at a rate of 100 per minute! The first blood vessels of the circulatory system appear. The appendix and pancreas are now evident, and inside the mouth, tooth buds, a tongue and the palate are all developing.
Pregnancy Checklist at 7 Weeks
- Book your private early pregnancy scan: Clear 7-week scan images can provide valuable information about your baby’s development and well-being. Ultrasound scans, especially the Viability Scan, offer emotional moments for expectant parents, providing a tangible connection to their growing baby and reassurance about their well-being. Despite natural concerns or anxieties, these routine and safe procedures offer valuable insights into the baby’s development.
- Monitor your health and well-being: As your baby continues to grow rapidly, take care of yourself by maintaining a healthy lifestyle, eating nutritious foods, and staying active as recommended by your healthcare provider.
- Keep an eye on your nutrition: Keep focusing on foods supporting fetal development and ensuring you get essential vitamins and minerals.
- You’re not alone, talk to professionals: During the early stages of pregnancy, it’s crucial to communicate with your healthcare provider as your hormones and body begin to change. They can offer guidance, support, and reassurance for any questions or concerns. Your provider has the expertise to address any issues or uncertainties that may arise, so don’t hesitate to reach out to them whenever needed.
Developmental Milestones: Week 7
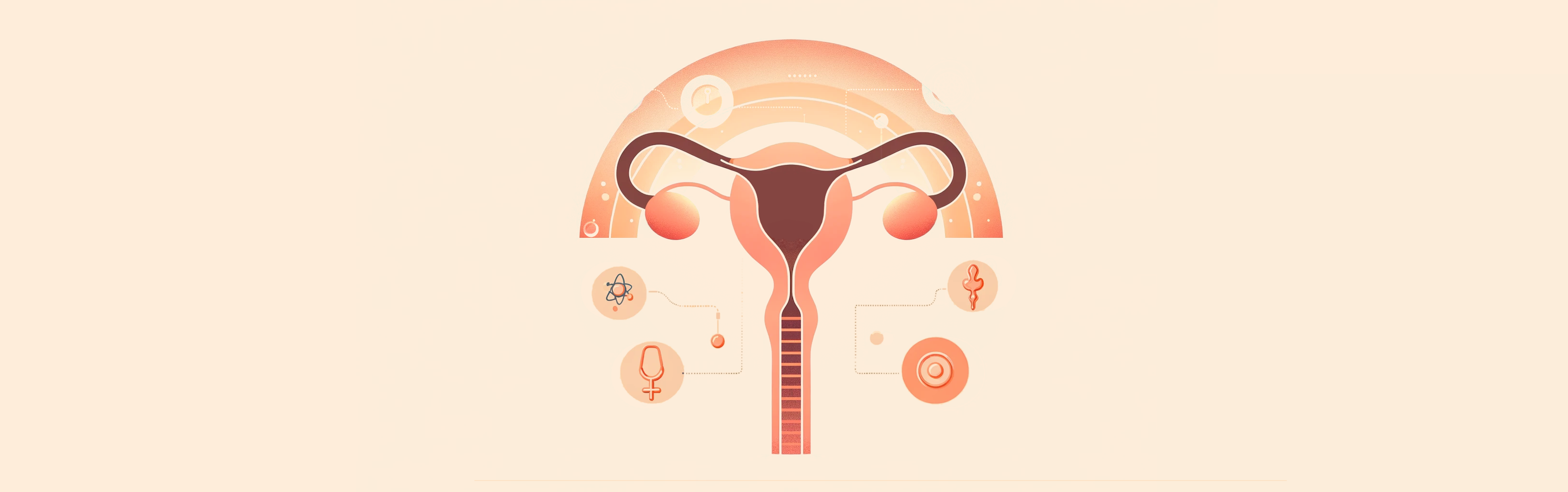
Embryonic Growth: The embryo now measures between 9mm to 10mm long (from crown to rump – CRL) and is 10,000 times bigger than it was at conception. Your baby’s fingers and toes are now formed, although not separated, giving them a paddle-like appearance. The embryo shows flurries of rapid movements at this stage. The liver is now producing red blood cells, and will continue to do so until bone marrow is formed which then takes over the production of red blood cells.
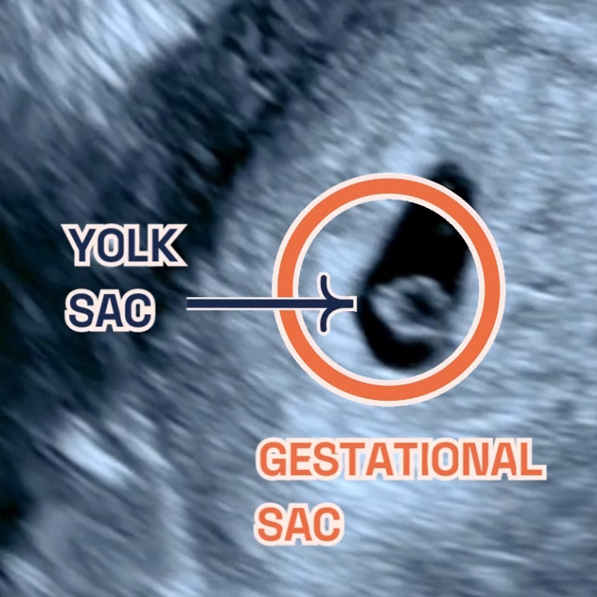
Gestational and Yolk Sac Development: At 7 weeks the gestational sac typically ranges from 18 to 25 mm. The yolk sac is about 3 mm. Both continue to grow steadily. The yolk sac provides nutrients and aids in blood cell formation until the placenta takes over this role. In Week 7, the gestational and yolk sacs play a critical role in your baby’s development. The gestational sac envelops the embryo, but its presence doesn’t guarantee a normal, healthy pregnancy. An anembryonic pregnancy, or blighted ovum, may occur, where the gestational sac lacks an embryo. This can be caused by various factors. If they are significantly smaller, it may indicate a potential first-trimester pregnancy loss. Seek guidance from early pregnancy specialists and obstetric professionals for further evaluation and support.
Heart Development: Between weeks 6 and 7 of pregnancy, the baby’s heart rate speeds up, usually ranging between 120 and 160 beats per minute.
Baby Features Development: By the end of week 6, the ears are continuing to form while the eyes are now covered with the beginnings of what will later become eyelids. Now at week 7, your baby’s fingers and toes are formed, although not separated, giving them a paddle-like appearance.
What is seen on the Ultrasound: Week 7?
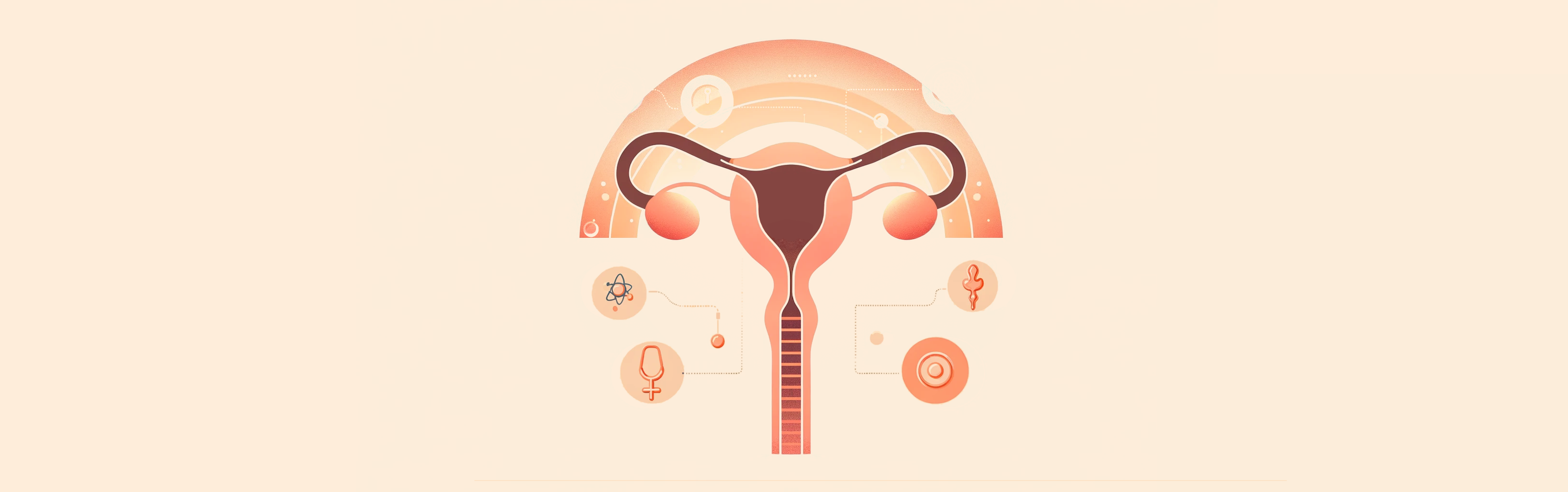
As you enter Week 7 of your pregnancy, the ultrasound offers a more intricate view of your baby’s development, building upon the observations from Week 6. This scan is a window into a world of rapid growth and transformation taking place within you. During the 7-week ultrasound, expect to see enhanced and more distinct images. The heartbeat, which was a delicate flicker last week, is now more pronounced and rhythmic, beating confidently as a testament to your baby’s vitality.
The gestational sac, your baby’s first nurturing environment, continues to grow, signifying healthy progression. Inside this protective sac, the yolk sac remains visible, providing essential nourishment. It’s a critical component until the placenta fully develops and takes over the role of supporting your baby.
The embryo itself is undergoing remarkable changes. Now resembling a tiny being with a more defined head and a tail-like structure, the embryo’s curved form is more noticeable. This is the period when major organs start forming. The healthcare provider may measure the embryo from head to tail, known as the CRL. Alongside, the size of the gestational sac is also measured, providing further information about the pregnancy’s progression.
This week’s ultrasound is pivotal for confirming the pregnancy’s viability, as it checks for the presence of a heartbeat and helps rule out any complications. Depending on the clarity needed, the ultrasound may be performed trans-abdominally or transvaginally, with the latter often providing a clearer view of these early developmental stages. Each pregnancy is unique, and these developmental milestones may vary slightly from one individual to another but what to expect during the ultrasound scan will remain the same.
-
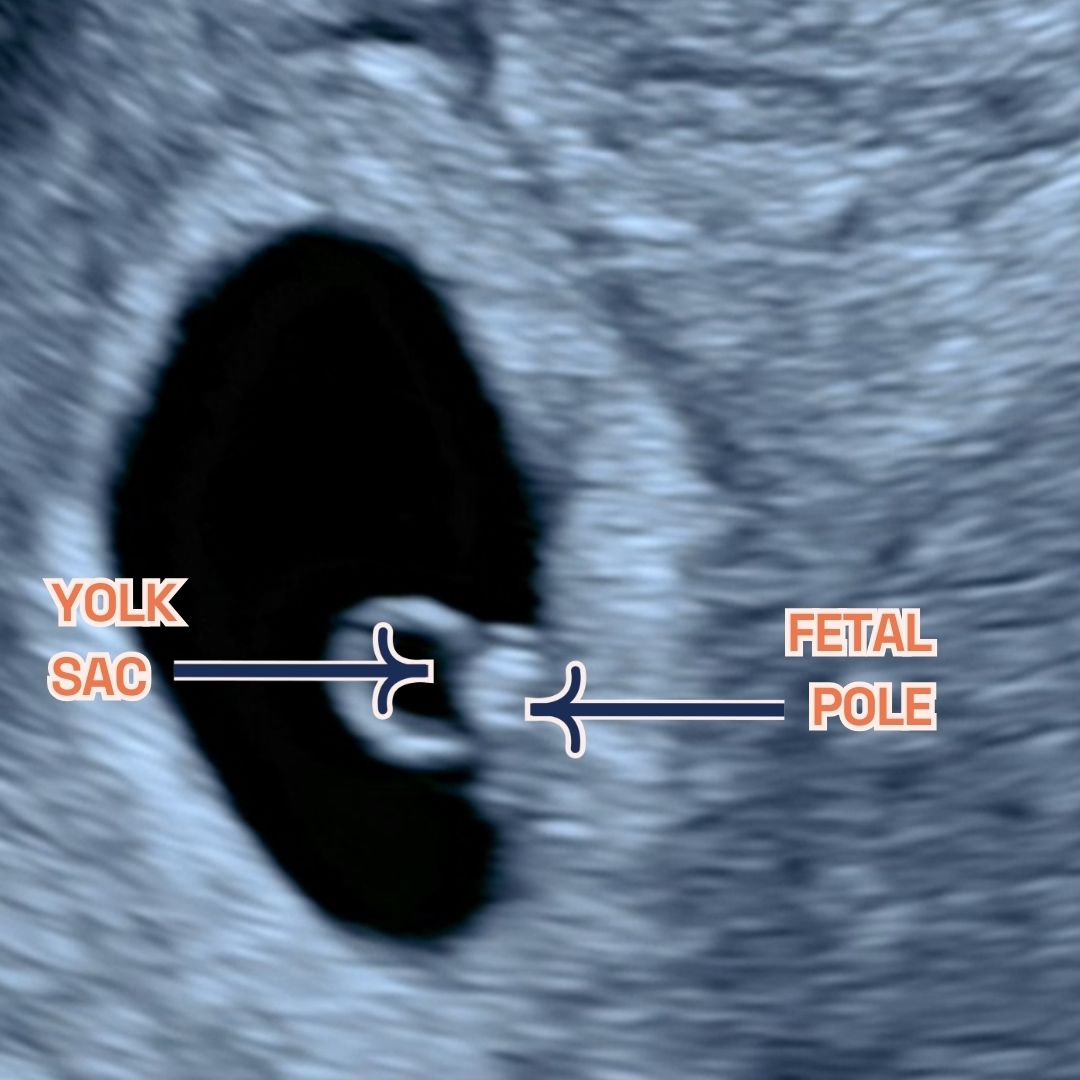
Gestational sac, fetal pole and yolk sac at 6 weeks of pregnancy as seen on ultrasound scan.
-
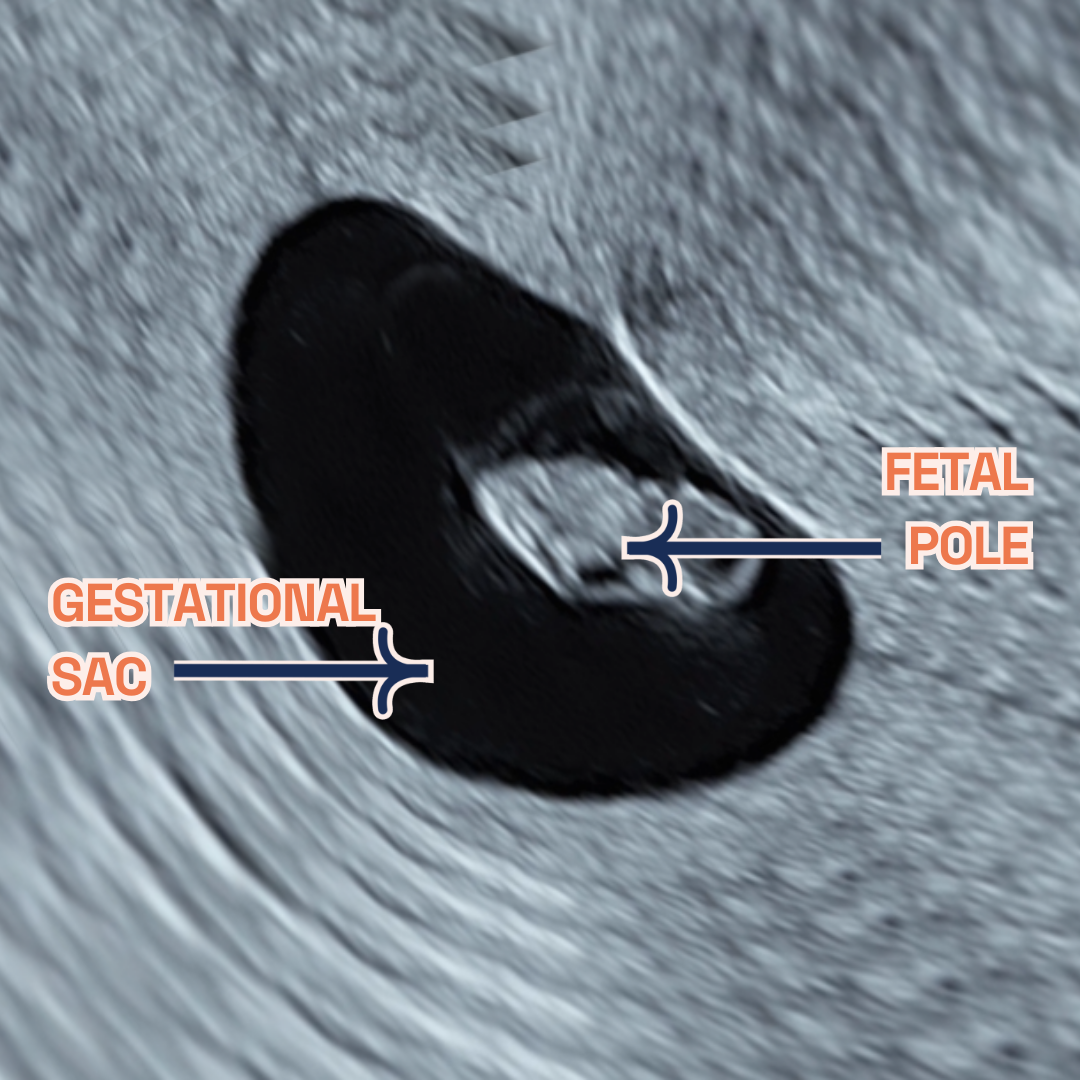
Gestational sac, fetal pole and yolk sac at 7 weeks of pregnancy as seen on ultrasound scan.
Thinking ahead: Week 8?
As you approach Week 8, expect further growth and development. Your next scan will provide more details about your baby’s progress. Keep following health guidelines and get ready for your next prenatal appointment. To support this critical growth phase, discuss upcoming screenings (we offer free counselling during our Viability Scan for NIPT) and nutritional adjustments with your healthcare provider. Approximately 75% of pregnant women experience morning sickness, which is a common symptom during week 7 of pregnancy. Rest assured, it’s a normal part of the journey. Despite its name, it can happen at any time of the day and is likely caused by hormonal changes and uterine muscle stretching. Nausea and vomiting usually improve between weeks 12 to 14 of pregnancy. Seek medical advice for severe morning sickness and remember, relief is on the way in a few weeks! Hang in there!
Conclusion
Week 7 of Pregnancy FAQs
-
How does 7 weeks pregnant look like?
At 7 weeks pregnant, your tiny miracle experiences remarkable growth!
- Baby development: This stage marks rapid progress. Your little one, roughly the size of a grape (around 9-10mm long), showcases significant development. The brain, crucial for future cognitive function, grows quickly, leading to a prominent forehead. Meanwhile, eyes and ears continue their formation, laying the groundwork for sight and hearing. Tiny limb buds, precursors to arms and legs, begin to transform into cartilage, the foundation for future bones. Nerve cells multiply rapidly, supporting your baby’s incredible growth spurt.
- Maternal experiences: As your baby thrives, your body adapts. The womb expands to accommodate your growing miracle, reaching around the size of a lemon. Common symptoms like fatigue, tender breasts, frequent urination, and morning sickness might arise, though remember, that every pregnancy is unique, and your experiences may differ.
Disclaimer: Remember, this information is for general knowledge only and should not be considered a substitute for professional medical advice. Always consult your healthcare provider for personalised guidance and to address any concerns you may have.
-
What to expect when 7 weeks pregnant?
As your baby flourishes, you may notice personal changes as well:
- Morning Sickness: A common symptom, though it doesn’t affect everyone.
- Fatigue: It’s normal to feel unusually tired as your body nurtures your growing baby.
- Sore Breasts: Hormonal changes may cause tenderness or swelling.
- Food Preferences: You might find your taste preferences changing.
- Enhanced Sense of Smell: Scents may become more intense.
- Mood Fluctuations: Hormones can lead to emotional variability.
Additional experiences some women report include:
- Metallic Taste: An odd but temporary sensation.
- Headaches: Ensure you’re well-hydrated and consult a doctor if headaches are frequent.
- Light Spotting: While it may be alarming, it’s not always a sign of trouble. Seek advice from your healthcare provider for reassurance.
- Cramps: These can resemble period pains but are generally less severe.
Advice to Remember:
- Stay Hydrated: Drinking water is crucial for your changing body.
- Maintain a Healthy Diet: A balanced diet benefits both you and your baby.
- Listen to Your Body: Rest as necessary and focus on self-care.
- Seek Support: For any concerns, professional guidance from your healthcare provider is invaluable.
Each pregnancy journey is distinct. Embrace this special time and the transformations it brings.
-
Can you feel movement seven weeks of pregnancy?
At 7 weeks into pregnancy, feeling your baby’s movements is usually too soon. Typically, the initial signs of fetal movement, or quickening, are experienced between 13-25 weeks, with some noticing these sensations as early as 13-16 weeks. Initially described as a flutter, these movements can be subtle, often mistaken for gas or similar sensations. The timing of when these movements are felt can be influenced by various factors, including the placenta’s position, the volume of amniotic fluid, and the mother’s body mass index. However, at week 8 of pregnancy, the baby starts moving inside the womb and that can be seen during an ultrasound scan.
-
I am bleeding when I’m 7 weeks pregnant – what do i do?
Prompt medical attention is crucial for bleeding at 7 weeks of pregnancy. Light spotting may not always be concerning, but professional consultation is essential to rule out serious conditions such as miscarriage or ectopic pregnancy. Immediately contact your midwife or GP, especially if accompanied by severe pain or dizziness, for assessment and appropriate care.
Note: This is educational content and not medical advice. Consult your healthcare provider for any pregnancy-related concerns, especially bleeding.
-
I am having twins during my 7 weeks viability scan
Discovering you’re expecting twins at your 7-week viability scan is a possibility, thanks to the precision of modern ultrasound technology. Particularly, a transvaginal ultrasound can effectively identify twins as early as 6 weeks into pregnancy. This type of scan can reveal the presence of multiple gestational and yolk sacs, fetal poles, and even distinct heartbeats, all indicative of a twin pregnancy. Notably, during the 7-9 week period, transvaginal ultrasounds are highly reliable for assessing the specifics of twin pregnancies, such as chorionicity and amnionicity.
Conclusion
Week 7 is a period of significant progress in your pregnancy. London Pregnancy Clinic is here to support you with expert care and detailed scans. Remember, every pregnancy is unique, so embrace your journey with confidence and excitement. Stay tuned for our next update as you continue this incredible journey.
Stay tuned on what your baby’s week-by-week growth will look like on our blog.